Inauguration Day solidifies the latest harrowing attack on Americans’ reproductive rights in the swearing in of President-elect Donald Trump.
The incoming president challenged1 the constitutional right to abortion afforded to American women by Roe v. Wade during his campaign and has reaffirmed his intent to appoint a pro-life Supreme Court justice since his election.2 In a November 60 Minutes interview,3 journalist Lesley Stahl questioned Trump on his stance of overturning Roe v. Wade, asserting that if the right was overturned federally, some women would not be able to get an abortion. He responded, “It’ll go back to the states. They’ll perhaps have to go, they’ll have to go to another state.”
Trump has also sent mixed messages on his support for/opposition to health care providers such as Planned Parenthood and intentions to overturn—at least parts of4—the Affordable Care Act5 (ACA), which has provided 47 million American women with access to guaranteed preventive health care.6 ACA enrollment has also specifically reduced the proportion of uninsured women of reproductive age (15–44) by 36 percent during its first two full years of implementation from 2013 to 2015.7
Of course, lawmakers in federal- and state-level legislatures have only substantiated the assault on reproductive care. Just a few weeks into their 2017 session, Republican lawmakers are making good on their intentions to “repeal and replace” the ACA, beginning with a Senate procedural vote on January 128—although concrete replacement plans remain unclear;9 Speaker Paul Ryan (R-WI) declared on January 5 that Congress’s ACA repeal would encompass legislation to defund Planned Parenthood.10

Last month, the state of Texas approved new rules—which took effect December 19—that mandate fetal remains to be buried or cremated like a deceased person.11 This winter has also witnessed the congressional passage of what is arguably the most extreme anti-abortion law nationwide, Ohio’s “Heartbeat Bill”—which sought to ban abortion in all cases after a heartbeat can be detected (about six weeks into a pregnancy).12 Though this bill was vetoed by Governor John Kasich, he did further limit Ohio women’s access to abortion by decreasing the legal time limit to undergo the procedure to just twenty weeks. 13And in Missouri, medically unnecessary restrictions are so stringent that just one licensed abortion provider remains open—statewide.14
With developments stemming from the 2016 election cycle clearly only the latest in terms of a long history of reproductive rights continuously being under fire, many Americans are concerned about women’s access to safe and affordable abortion and family planning services as well as contraceptives. Looking ahead to the next administration, it is imperative to understand just how limited access to reproductive care already is for many American women, especially low-income women, and just how many barriers they face in attempting to reach those access points on all levels of governance. This report analyzes these disparate access points and barriers to reproductive care for women in different states, honing in on abortion services. It also offers immediate state and nonprofit action that can be taken to enhance and defend this care as reproductive rights enter yet another age of assault.

Who Gets Abortions?
It is worth emphasizing that despite abortion being at the center of a heated ideological debate for decades, no one abortion story is the same.15 Along these same lines, thanks to data put forth by the Guttmacher Institute,16 the demographic makeup of American women getting abortions is also quite varied. In terms of age, in 2014, the majority of abortions—59 percent—were obtained by mothers who already had a child. Only 12 percent of abortion patients were teenagers, while over half were in their 20s. Also in 2014, white patients comprised 39 percent of American abortions, blacks 28 percent, Hispanics 25 percent, and other races/ethnicities accounting for 9 percent of abortions. The religious breakdown of abortion patients that year showed us that 17 percent called themselves mainline Protestant, 13 percent identified as evangelical Protestant, 24 percent were Catholics, and 38 percent stated no religious affiliation.17 Forty-nine percent of all these patients had incomes lower than that of the federal poverty level.18
A Guttmacher study, “Reasons U.S. Women Have Abortions: Quantitative and Qualitative Perspectives,” stated that over three-quarters of surveyed patients gave three most common reasons for obtaining abortions: “Concern for or responsibility to other individuals; the inability to afford a child; and the belief that having a baby would interfere with work, school or the ability to care for dependents.” Additionally, half of those surveyed stated that “they did not want to be a single parent or were having problems with their husband or partner.”19
Where Do We Stand with the Law and Policy Today?
The landmark Supreme Court case of Roe v. Wade (1973)20 ruled that under the Fourteenth Amendment’s Due Process Clause, all American women have the right to make their own decisions about abortion prior to viability without interference from the state. The court in Roe left the question of regulation during the third trimester of pregnancy to the states. Planned Parenthood of Southeastern Pennsylvania v. Casey (1992)21 challenged this third trimester provision and successfully altered the legal timeframe to be in accordance with fetal viability; the court—in addition to upholding Roe’s “essential holding” of a woman’s right to choose—also ruled that “abortion restrictions could not impose an undue burden on a woman seeking to terminate her pregnancy” in Casey.
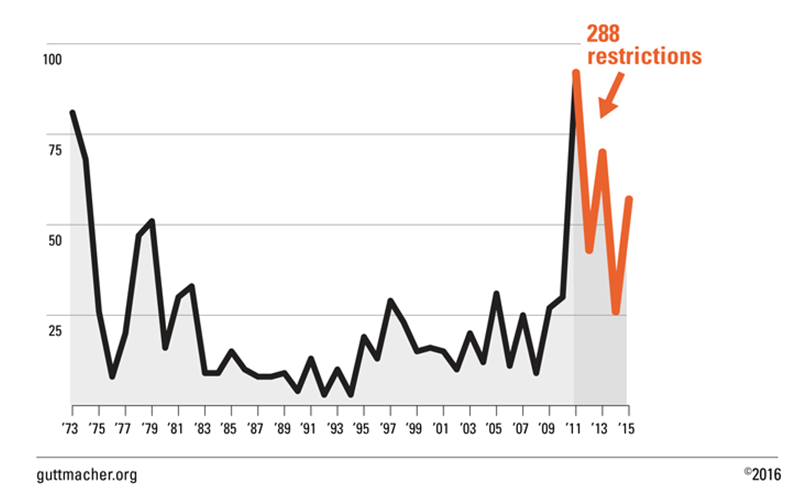
States therefore had more freedom to regulate abortions in that they could determine—for themselves—the meanings of the loosely legally defined “viability” and “undue burden” as they saw fit. And so they did: states have enacted 1,074 abortion restrictions since Roe, with upticks seen throughout the 1990s following Casey and even more dramatically, after the 2010 midterm elections, in which many pro-life congressional representatives were elected (see Figure 1). In fact, the 334 abortion restrictions enacted by states in the past five years have accounted for 30 percent of all abortion restrictions in the past forty-three years since Roe.22
In 2016 alone, 1,256 provisions regarding sexual/reproductive health and rights have been introduced by legislators; 445 of these provisions seek to inhibit access to abortion services. Fifty new abortion restrictions were passed by eighteen different states.23 Also in 2016, thirty-two states attempted to ban all or some abortions. Four states (Alabama, Louisiana, Mississippi, West Virginia) have enacted measures to ban the most common method used to perform abortions during the second trimester—dilation and evacuation (D&E). Mississippi and West Virginia’s laws are in effect; Alabama’s and Louisiana’s are currently challenged in court. Similar legislation has been introduced in sixteen states.24
After Texas put forth some of the toughest abortion restrictions nationwide with House Bill 2,25 the Supreme Court struck down said inhibitions26 and upheld Casey in Whole Woman’s Health v. Hellerstedt (2016).27 The court furthermore defined “undue burden” by stating:
“We begin with the standard, as described in Casey. We recognize that the “State has a legitimate interest in seeing to it that abortion, like any other medical procedure, is performed under circumstances that insure maximum safety for the patient.” Roe v. Wade, 410 U. S. 113, 150 (1973). But, we added, “a statute which, while furthering [a] valid state interest, has the effect of placing a substantial obstacle in the path of a woman’s choice cannot be considered a permissible means of serving its legitimate ends.” Casey, 505 U. S., at 877 (plurality opinion). Moreover, “[u]nnecessary health regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.”
Also in 2016, Oklahoma Governor Mary Fallin—a conservative Republican who has supported numerous abortion restrictions in her state—struck down28 a bill passed by the state legislature that would have effectively banned abortion in the state by imposing felony charges on doctors who perform such procedures.29 She called the bill unconstitutional, adding that the way to overturn Roe v. Wade would be “the appointment of a conservative, pro-life justice to the United States Supreme Court.”30
And on December 31, 2016, the U.S. District Court for Northern Texas ruled in Franciscan Alliance v. Burwell that on the basis of religious freedom, doctors can refuse to treat women who have had abortions as well as transgender patients.31
For Reproductive Rights, Not All States Are Created Equal
As the aforementioned state challenges to a federally guaranteed constitutional right imply, women’s access to abortion services and reproductive care is starkly different depending on where it is they call home.
Access: Where Can American Women Get Abortions?
In 1981, approximately 2,900 facilities nationwide legally provided abortion services.32 That number has declined dramatically to roughly 1,700 providers as of 2011. However, these raw numbers do not tell the whole story: In 2008, while hospitals comprised 34 percent of all American abortion facilities, they only actually performed 4 percent of all abortion procedures. Nineteen percent of abortion providers were physicians’ offices, but they were responsible for just 1 percent of abortions. Meanwhile, though clinics comprise only 47 percent of all abortion facilities, they performed 94 percent of recorded abortions nationwide. This data forced Guttmacher Institute researchers Rachel K. Jones and Jenna Jerman to assert, “Provider type, and the number of clinics in particular, may be a more important indicator of access than the total number of providers.”33
As of 2011, 89 percent of U.S. counties did not have an abortion clinic.34 This means that, of the United States’ 3,143 counties or county equivalents,35 2,797 lacked abortion clinics. Thirty-eight percent of reproductive age women lived in these counties.36 Digest that: over a third of Americans do not have basic access to obtaining a procedure that is federally afforded to them as a constitutional right. Of the 346 counties that do have clinics with abortion services, Planned Parenthood centers are the leading abortion providers.
As Guttmacher has estimated, of the 491 U.S. counties that have Planned Parenthood centers, in 332 of them, Planned Parenthood centers served at least half of all safety-net family planning centers, which provide contraceptive care to the general public at a free or reduced price by using public funds.37 In 103 of these counties, Planned Parenthood centers are the only safety-net family planning centers available whatsoever.38
The Century Foundation (TCF) has taken this investigation one step further: many Planned Parenthood centers do not offer abortion services, making the question of access points all the more dire. I have found that of the 662 Planned Parenthood centers open nationwide as of 2016,39 367 of them—55.44 percent—provide abortion services. Additionally, 255 of them—38.52 percent—offer abortion referral services. And 40 of them, concentrated in Louisiana, Texas, and Wisconsin—6.04 percent—offer neither abortion services nor abortion referral services, instead solely offering Planned Parenthood’s other services including general health care, pregnancy, HIV, and STD testing, and birth control. These data points on access to abortion are reflected in Map 1, juxtaposed against U.S. Census Bureau data for reproductive age women in each state (2015 estimates).40
The decision to include the distribution of the 204 non-Planned Parenthood, National Abortion Federation (NAF) member abortion providers (mostly clinics)41 in the map was made to demonstrate the dominance Planned Parenthood has over both physical access points to abortion procedures as well as access to reputable information on where one can safely obtain said abortions.42
Map 1. Number of Planned Parenthood/National Abortion Federation Abortion Providers, Per Population of Reproductive Age Women, By State
Sources: Compiled by author from “Planned Parenthood Health Centers by State,” Planned Parenthood, 2016; “Find A Provider,” National Abortion Federation, 2016; “American FactFinder: Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2015, 2015 Population Estimates,” United States Census Bureau, June 2016.
Note that the above map does not reflect the distance some women must travel to reach an abortion provider. The New York Times has created some graphics illustrating these distances for white, black, and Hispanic women in different states of different income levels.43
Barriers to Care
In addition to unequal access to abortion providers dependent on one’s home state, American women face numerous other state-mandated barriers to care. Table 1 illustrates the following barriers: state government-funded, mandated counseling/distributed materials; state restrictions on later abortion; state parental consent policies; state private insurance policies on coverage of abortion procedures; and whether states publicly fund abortion procedures or not.
A breakdown of state-imposed barriers to reproductive care across all fifty states and Washington, D.C can be found at the end of this piece.
Government-Mandated Counseling
Numerous states have mandates in place that require women seeking to obtain abortions to take part in counseling centering around various information meant to dissuade women from going through with the procedures.44 Five states45 have mandated counseling on the link between abortion and breast cancer (though the American Cancer Society declares that a cause-and-effect relationship between abortion and breast cancer has not been found46); twelve states require counseling on fetal pain; and nine states mandate counseling on negative psychological effects of abortion.47 Paired with various mandatory waiting periods and either offered or given distributed materials, these efforts can serve as a coercive barrier to care.48
Ultrasound Requirements
In thirteen states, women seeking abortions are required to receive (often costly) ultrasounds from their providers despite ultrasounds not being medically necessary during the first trimester. In three of these states, the provider must both display the image and describe it to the woman; in nine states, the provider has to give the woman the option to see the image, and in one, Oklahoma, the provider does not have to ask the woman whether or not they’d like to see the image following the ultrasound procedure. In some states women must also listen to detailed descriptions of the images; only in Virginia and Wisconsin are women not required to undergo the ultrasound procedure if they have been raped. In fourteen other states women are given either verbal and/or written information on how to access ultrasounds.49
State Restrictions on Later Abortion
Forty-three states have restrictions of some kind in place regulating later abortion. Of them, sixteen states have banned women from obtaining abortion beyond twenty weeks after fertilization; others measure between twenty and twenty-four weeks after the last menstrual period. Nineteen limit abortion after viability, which is the point at which a fetus is thought to be able to survive outside of the uterus.50 Viability is typically considered to be between the twenty-fourth and twenty-eighth weeks of pregnancy.51 Exceptions to these restrictions on later abortion include threats to the well-being or life of the mother, as well as cases of rape or incest.
Parental Consent Policies
Thirty-seven states mandate some form of parental consent or notice in the case that a minor attempts to obtain an abortion. Seventeen require consent of a parent, ten require that a parent be notified of the procedure. Two require that both parents be notified; four require that both parents give their consent; and four require that both parents be notified and both give their consent.52 Stricter laws on this front can be damaging to a pregnant young woman (who may have ideologically pro-life parents unwilling to give consent, or perhaps a parent that lives geographically far away and cannot readily provide a signature of consent) given the critical nature of timeliness when it comes to abortions. Time is even more of the essence in states that have more imposing later abortion restrictions (which as Table 1 shows, often coincide with those states with stricter consent laws) and in states that have fewer clinics—meaning waiting lists for procedures are longer.
Private Insurance Policies, Health Care
The Hyde Amendment53—passed by Congress in 1976 and attached to appropriations bills annually since then—prohibits the use of federal funds for abortions except in the cases of rape, incest, or the endangerment of a woman’s life.54 This means that health insurance provided by the federal government such as Medicaid cannot cover abortions under other circumstances.55 States can, however, choose to use their own funds to cover these abortions—but at this point, just seventeen states publicly fund abortion procedures (other than in the aforementioned three exceptional circumstances). South Dakota will fund abortions only in the case of the mother’s life endangerment. Thirty-two states and Washington, D.C. can rely on public funding only as covered by the federal Hyde provisions.56 Furthermore, twenty-five states ban coverage of abortion procedures in private plans through health insurance marketplaces.57
It is critical to acknowledge that these limitations on insurance coverage further substantiate abortion as an equity issue. Though women from all different socioeconomic backgrounds obtain abortions, those who are low-income (as half of patients are58) are hit hardest by attacks on reproductive care. After all, in 2014, 53 percent of all recorded abortion patients were forced to pay out of pocket for their procedures.59
Restricting Public Funding for Family Planning, Contraception, and Related Care
The Title X Family Planning Program, enacted in 1970, allocates federal funds to states for distribution to organizations like Planned Parenthood that provide contraception and other non-abortion-related family planning services.60
Many states have tried to restrict organizations’ eligibility for Title X funds on the basis of whether the organization at hand also provides abortion services. From July 2015 to July 2016 alone, twenty-four states attempted to do so.61
By blocking funding to family planning organizations, states are depriving women of critical health care. It’s important to remember that just 3 percent of Planned Parenthood’s overall services are abortions among the myriad of other types of care they provide, including: contraceptive care, preventing unintended pregnancies, pap tests, breast exams, STI treatment and HIV tests, and educational programs and outreach.62
It’s also unconstitutional. In September, President Obama put forth a rule change63 that would prevent states from withholding funds—including Title X funds and Medicaid reimbursements for lower-income patients—from organizations for any reason other than their inability to effectively provide these services (including if that organization also provides abortion services).64 After a lengthy public comment period conducted by the Department of Health and Human Services in which 91 percent of respondents were in favor, the law was rendered final on December 14. It went into effect on January 18, 2017—two days before President-elect Trump takes office.65 A joint bill of disapproval from both houses of Congress and the president have the power to reverse the decision.
Harassment Outside of Abortion Provider Clinics
Unfortunately, harassment outside of abortion providers can also deter many women from obtaining abortion procedures. While many states have buffer zones in place to prevent this kind of harassment, this is not the case across much of the United States—even in progressive Massachusetts, Supreme Court case McCullen v. Coakley (2014) overturned Massachusetts’ thirty-five-foot buffer zone law around reproductive health clinics.66
Abortion Safety
Abortions performed the right way are safe—first-trimester abortions have just a .05 percent risk of major complications67—but restricting access forces women to undergo unsafe procedures in the shadows.
Olga Khazan of The Atlantic speaks to these dangers in a recent article covering conditions for Texan women seeking abortions between House Bill 2’s implementation in 2013 and its recent shutdown by the Supreme Court.68 The University of Texas’s Texas Policy Evaluation Project found that women whose nearest abortion clinic had been closed due to the legislation faced, on average, an eighty-five-mile commute to receive abortion care.69 They also conducted a survey that found between 100,000 and 240,000 women in Texas had or had tried to induce their own abortions. As Khazan writes,
“The most common method reported was by taking the drug Misoprostol, also known by the brand name Cytotec. Other reported methods included ‘herbs or homeopathic remedies, getting hit or punched in the abdomen, using alcohol or illicit drugs, or taking hormonal pills.’”70
Contraceptive Care
While the attack on organizations like Planned Parenthood might be driven by pro-life, anti-abortion idealists, it’s worth noting—as access to contraceptive care and abortions are inherently linked—that 80 percent of Planned Parenthood patients are receiving services to prevent unintended pregnancies.71

As a large part of accessibility can be affordability, access to contraceptive care would also be severely impacted by an overturn of the ACA, which made many forms of birth control free under both marketplace and private insurance plans.72 Direct threat to this provision has been heightened by Trump’s recent appointment of Representative Tom Price (R-GA) as health secretary, a critic of abortion practices who has been both a vocal opponent of the ACA and a supporter of barring federal funding to Planned Parenthood,73 as well as Senate Republicans’ procedural vote against a proposed amendment to preserve free contraception with an ACA repeal on January 12.74
Positively, in 2016, many states took legislative action to preserve and expand insurance coverage for contraceptive care:75 following Maryland’s bill passed in 2015,76 thirteen states put forth legislation guaranteeing full coverage of contraceptives; six states introduced bills providing coverage for over-the-counter methods of birth control; nine states proposed expanding coverage of sterilization; and seventeen states put forth bills allowing people to be granted up to a year’s supply of birth control at once.77 In 2016, both Oregon and California implemented legislation enabling their residents to obtain birth control without prescriptions.78 Hawaii also notably became the first state to require all insurers to cover up to a year-long supply of birth control.79
Key Fronts in the Struggle Ahead
While these recent protections and expansions of contraceptive care accessibility are critically beneficial, they do not serve Americans in all states—demonstrating, in line with America’s history of reproductive health, that access to care is determined by an individual’s zip code or resources at hand.
For American women seeking reproductive health care with restrictive laws in place, particularly those of lower socioeconomic status, the existence of Roe v. Wade is the not just the last, but essentially the only, line of defense. If it is overturned after the appointment of a pro-life Supreme Court justice, women in nineteen states that already have pre-1973 laws in effect would immediately be prevented from getting abortions.80
Had Hillary Rodham Clinton won the presidency and appointed a progressive Supreme Court justice, the path for addressing state-by-state inequities with regard to access and barriers to reproductive health care would have been clear. Given the realities of the Trump administration, and the likelihood that the provision of reproductive care will becoming increasingly worse in many states, activists, health providers, and members of state government who want to preserve reproductive health care must instead play defense, protecting whatever access currently exists—particularly in states where legislatures are intent on eliminating critically important services.
State-level Action
State legislators can mandate insurers to cover birth control without co-pays. While it should be obvious, reducing the cost of birth control will also reduce the number unintended pregnancies, and thus the need for abortion procedures.81 Maryland is at the forefront of states that already do this,82 having passed “the most sweeping birth control access law” this year.83 California and Illinois also require insurance plans to cover contraception at no cost. Vermont has enacted a similar law, and many other states have introduced legislation to provide their citizens with the same access to truly free birth control. As noted by leading reproductive rights organization NARAL, this kind of state-level legislation will be particularly important should the ACA be repealed.84 The aforementioned measures taken by states such as Oregon, California, and Hawaii allowing women to access contraceptives without prescriptions and to pick up bulk quantities of birth control further increase access to care.
In addition to putting forth legislation improving contraceptive access, states should protect and enhance family planning funds. The Montana state legislature passed a bipartisan bill moving Title X funds from the congressional budget process and safely into statute. These family planning funds will now be administered solely by the Department of Public Health and Human Services, meaning that state legislatures cannot vote to withhold Title X funds from family planning centers on the basis that the centers also provide abortion services.85
Nonprofit Action
Civil and reproductive rights groups with litigation teams could prove to be exceptionally important over the course of the next few years.
On November 30, Planned Parenthood, the American Civil Liberties Union (ACLU), and the Center for Reproductive Rights joined together in filing simultaneous lawsuits challenging excessive and medically unecessary abortion restrictions in Alaska, North Carolina, and Missouri—the lattermost so extreme that there is just one licensed abortion provider still open statewide.86 Director of the ACLU’s Reproductive Freedom Project Jennifer Dalven said of the wave of litigation,
“Because of laws like the ones we are challenging today, for too many women across our country the constitutional right to have an abortion is more theoretical than real. With the cases we are filing today, we are sending a clear message that we won’t stop working until every woman can get the care she needs no matter who she is, where she lives, or how much money she makes.”87
Attorneys from all three organizations are representing the various plaintiffs involved in the three cases. The ACLU has additionally filed class action for a plethora of the aforementioned state barriers to abortion care ranging from fighting an Arizona law attempting to exclude abortion providers from the state’s Medicaid program88 to successfully challenging Alabama laws that would have forced abortion clinics within certain proximity to schools to close, as well as banned safe procedures for abortions during the second trimester.89
Beyond putting forth litigation defending reproductive rights, these organizations are already channeling public support galvanized by the election cycle and its results toward grassroots organizing efforts—ranging from sponsorship of the Women’s March on Washington90 to continued training programs91 for citizens seeking to influence change within their communities by volunteering as abortion escorts, for example. Right now, public sentiment is heavily in favor of preserving access: Pew Research Center found in December that significantly more Americans today—69 percent (72 percent of women and 67 percent of men)—than in the past (63 percent in 2013) believe that Roe v. Wade should not be repealed.92
Despite a strong majority public opinion, this fight has typically occurred along party lines.93 With the Republican Party now controlling both houses of Congress and the White House (and thus, shortly, tipping the Supreme Court in their favor) nonprofit groups using the law and their organizing power seems to be the strongest avenue for defending access to reproductive care and demanding justice for American women.
Editor’s note: Though this report focuses on access to abortion services at Planned Parenthood centers, it was written independently of Planned Parenthood.
Additionally, as pointed out by Guttmacher Institute research published in January 2017, the number of abortion restrictions enacted since 2010 is now 338 (their updated graphic can be found here); also this month, Guttmacher found that the percent of United States counties without a clinic was 90 percent in 2014 (this report uses 2011 data, which had this statistic at 89 percent).
CORRECTION: Map 1 has been updated as of 5 pm EST on January 19, 2017 to accurately reflect each state’s population of reproductive age women divided by Planned Parenthood and National Abortion Federation members offering abortion services, rather than total number of Planned Parenthood centers and National Abortion Federation members.
Acknowledgements
The author would like to thank The Century Foundation team for their support on this report—especially Julie Kashen and Jason Renker for their guidance, suggestions, and edits; as well as Simon Glenn-Gregg for skillfully designing the map.
State Barriers to Care Table
| Table 1. Barriers to Abortion Care by State | ||||||
| Government Mandated Counseling | Ultrasound Required? | State Restrictions on Later Abortion | Parental Consent Policy | Coverage of Abortion Procedures in Private Plans through Health Insurance Marketplaces | Public Funding of Abortion Procedures | |
| Alabama | Yes: provider must offer the woman the option to view the image | 20 weeks post fertilization | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Alaska | Yes: Breast Cancer Link, Fetal Pain | Funds all or most medically necessary abortions (State funded) | ||||
| Arizona | Yes: provider must offer the woman the option to view the image | Limit on abortion after viability | Consent | Bans marketplace coverage | Funds all or most medically necessary abortions (State funded) | |
| Arkansas | Yes: Fetal Pain | 20 weeks post fertilization | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| California | Limit on abortion after viability | Funds all or most medically necessary abortions (State funded) | ||||
| Colorado | Notice | Funds limited to life endagerment, rape, and incest (Federally funded) | ||||
| Connecticut | Limit on abortion after viability | Funds all or most medically necessary abortions (State funded) | ||||
| Delaware | Limit on abortion after viability | Notice, though health professional can waive | Funds limited to life endagerment, rape, and incest (Federally funded) | |||
| Florida | Yes: provider must offer the woman the option to view the image | 24 weeks after Last Menstrual Period (LMP) | Notice | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Georgia | Yes: Fetal Pain | 20 weeks post fertilization | Notice | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Hawaii | Limit on abortion after viability | Funds all or most medically necessary abortions (State funded) | ||||
| Idaho | Limit on abortion after viability | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| Illinois | Limit on abortion after viability | Notice | Funds all or most medically necessary abortions (State funded) | |||
| Indiana | Yes: Fetal Pain | 20 weeks post fertilization | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Iowa | 3rd trimester LMP | Notice | Funds limited to life endagerment, rape, and incest (Federally funded) | |||
| Kansas | Yes: Breast Cancer Link, Fetal Pain, Negative Psychological Effects | Yes: provider must offer the woman the option to view the image | 22 weeks LMP | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) |
| Kentucky | Limit on abortion after viability | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| Louisiana | Yes: Fetal Pain, Negative Psychological Effects | Yes: provider must display and describe the image | 20 weeks post fertilization | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) |
| Maine | Limit on abortion after viability | Funds limited to life endagerment, rape, and incest (Federally funded) | ||||
| Maryland | Limit on abortion after viability | Notice | Funds all or most medically necessary abortions (Federally funded) | |||
| Massachusetts | 24 weeks post implantation | Consent | Funds all or most medically necessary abortions (State funded) | |||
| Michigan | Yes: Negative Psychological Effects | Limit on abortion after viability | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| Minnesota | Yes: Fetal Pain | Limit on abortion after viability | Notice of both parents | Funds all or most medically necessary abortions (State funded) | ||
| Mississippi | Yes: Breast Cancer Link | Yes: provider must offer the woman the option to view the image | 20 weeks LMP | Consent of both parents | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) |
| Missouri | Yes: Fetal Pain | Limit on abortion after viability | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest | |
| Montana | Limit on abortion after viability | Notice | Funds all or most medically necessary abortions (State funded) | |||
| Nebraska | Yes: Negative Psychological Effects | 20 weeks post fertilization | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Nevada | 24 weeks post fertilization | Funds limited to life endagerment, rape, and incest (Federally funded) | ||||
| New Hampshire | Notice | Funds limited to life endagerment, rape, and incest (Federally funded) | ||||
| New Jersey | Funds all or most medically necessary abortions (State funded) | |||||
| New Mexico | Funds all or most medically necessary abortions (State funded) | |||||
| New York | 24 weeks post fertilization | Funds all or most medically necessary abortions (State funded) | ||||
| North Carolina | Yes: Negative Psychological Effects | Yes: provider must offer the woman the option to view the image | 20 weeks LMP | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) |
| North Dakota | 20 weeks post fertilization | Consent of both parents | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| Ohio | Yes: provider must offer the woman the option to view the image | Limit on abortion after viability *New 20-week ban passed in December, court has 90 days to challenge | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Oklahoma | Yes: Breast Cancer Link, Fetal Pain | Yes: provider not required to offer the option to view | 20 weeks post fertilization | Consent and notice | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) |
| Oregon | Funds all or most medically necessary abortions (State funded) | |||||
| Pennsylvania | 24 weeks LMP | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| Rhode Island | 24 weeks LMP | Consent | Funds limited to life endagerment, rape, and incest (Federally funded) | |||
| South Carolina | 20 weeks post fertilization | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| South Dakota | Yes: Fetal Pain, Negative Psychological Effects | 20 weeks post fertilization | Notice | Bans marketplace coverage | Life only | |
| Tennessee | Limit on abortion after viability | Consent | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | ||
| Texas | Yes: Breast Cancer Link, Fetal Pain, Negative Psychological Effects | Yes: provider must display and describe the image | 20 weeks post fertilization | Consent and notice | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Utah | Yes: Fetal Pain, Negative Psychological Effects | Limit on abortion after viability | Consent and notice | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Vermont | Funds all or most medically necessary abortions (State funded) | |||||
| Virginia | Yes: provider must offer the woman the option to view the image | 3rd trimester LMP | Consent and notice | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Washington | Limit on abortion after viability | Funds all or most medically necessary abortions (State funded) | ||||
| West Virginia | Yes: Negative Psychological Effects | 22 weeks LMP | Notice of both parents | Funds all or most medically necessary abortions (State funded) | ||
| Wisconsin | Yes: provider must display and describe the image | 20 weeks post fertilization | Consent of both parents | Bans marketplace coverage | Funds limited to life endagerment, rape, and incest (Federally funded) | |
| Wyoming | Limit on abortion after viability | Consent of both parents | Funds limited to life endagerment, rape, and incest (Federally funded) | |||
| Washington, D.C. | Funds limited to life endagerment, rape, and incest (Federally funded) | |||||
| Source: Compiled by author from “State Policies on Later Abortions,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/state-policies-later-abortions; “An Overview of Abortion Laws,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/overview-abortion-laws; Kinsey Hasstedt, “Abortion Coverage Under the Affordable Care Act: Advancing Transparency, Ensuring Choice and Facilitating Access,” Guttmacher Institute, April 9, 2015, https://www.guttmacher.org/about/gpr/2015/04/abortion-coverage-under-affordable-care-act-advancing-transparency-ensuring-choice; “Requirements for Ultrasound,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/requirements-ultrasound. | ||||||
Notes
- Monique Scotti, “Presidential Debate 2016: Donald Trump Says Overturning Roe v. Wade Will Happen ‘Automatically’,” Global News, October 19, 2016, http://globalnews.ca/news/3014304/presidential-debate-2016-donald-trump-says-overturning-roe-v-wade-will-happen-automatically/.
- Lesley Stahl, “President-Elect Trump Speaks to a Divided Country on 60 Minutes,” CBS News, November 13, 2016, http://www.cbsnews.com/news/60-minutes-donald-trump-family-melania-ivanka-lesley-stahl/.
- Tania Kohut, “Donald Trump Stands by Campaign Promise to Overturn Roe v. Wade,” Global News, November 14, 2016, http://globalnews.ca/news/3065226/donald-trump-stands-by-campaign-promise-to-overturn-roe-v-wade/
- Lesley Stahl, “President-Elect Trump Speaks to a Divided Country on 60 Minutes,” CBS News, November 13, 2016, http://www.cbsnews.com/news/60-minutes-donald-trump-family-melania-ivanka-lesley-stahl/.
- Mark Zuckerman and Simon Glenn-Gregg, “Where Are the Millions of People Who Would Lose Health Care Coverage without the ACA?,” The Century Foundation, November 22, 2016, https://tcf.org/content/facts/millions-people-lose-health-care-coverage-without-aca/.
- “ObamaCare and Women: ObamaCare Women’s Health Services,” Obamacarefacts.com, http://obamacarefacts.com/obamacare-womens-health-services/.
- “Uninsured Rate Among Women of Reproductive Age Has Fallen More Than One-Third Under the Affordable Care Act,” Guttmacher Institute, November 17, 2016, https://www.guttmacher.org/article/2016/11/uninsured-rate-among-women-reproductive-age-has-fallen-more-one-third-under.
- Thomas Kaplan and Robert Pear, “Senate Takes Major Step Toward Repealing Health Care Law,” New York Times, January 12, 2017, https://www.nytimes.com/2017/01/12/us/politics/health-care-congress-vote-a-rama.html.
- Harold Pollack, “The Challenge of ‘Repeal and Replace’ for Trump,” The Century Foundation, December 6, 2016, https://tcf.org/content/commentary/challenge-repeal-replace-trump/.
- Mike DeBonis, “Planned Parenthood Would Lose Funding as Part of Obamacare Repeal, Ryan Says,” Washington Post, January 5, 2017, https://www.washingtonpost.com/news/powerpost/wp/2017/01/05/planned-parenthood-would-lose-funding-as-part-of-obamacare-repeal-ryan-says/?utm_term=.37de508c395c.
- Liam Stack, “Texas Will Require Burial of Aborted Fetuses,” New York Times, November 30, 2016, http://www.nytimes.com/2016/11/30/us/texas-burial-aborted-fetuses.html?rref=collection%2Fsectioncollection%2Fus&action=click&contentCollection=us®ion=stream&module=stream_unit&version=latest&contentPlacement=7&pgtype=sectionfront&_r=1.
- Jason Hanna, Dominique Debucquoy-Dodley, and Max Blau, “Ohio Passes ‘Heartbeat’ Abortion Bill; Leader Cites Trump’s Election,” CNN, December 7, 2016, http://www.cnn.com/2016/12/07/politics/ohio-abortion-bill/.
- Randy Ludlow, “Gov. John Kasich Vetoes Heartbeat Bill, Signs 20-Week Abortion Ban,” The Columbus Dispatch, December 13, 2016, http://www.dispatch.com/content/stories/local/2016/12/13/John-Kasich-acts-on-abortion-bills.html#.
- Dan Margolies, “Planned Parenthood Sues to Overturn Missouri Abortion Restrictions,” KCUR, November 30, 2016, http://kcur.org/post/planned-parenthood-sues-overturn-missouri-abortion-restrictions#stream/0.
- Catherine Pearson, “There’s No One Abortion Story,” Huffington Post, 2016, http://testkitchen.huffingtonpost.com/abortion/.
- “Induced Abortion in the United States,” Guttmacher Institute, September 2016, https://www.guttmacher.org/fact-sheet/induced-abortion-united-states#8.
- Jenna Jerman, Rachel K. Jones, and Tsuyoshi Onda, “Characteristics of U.S. Abortion Patients in 2014 and Changes Since 2008,” Guttmacher Institute, May 2016, https://www.guttmacher.org/report/characteristics-us-abortion-patients-2014.
- “Induced Abortion in the United States,” Guttmacher Institute, September 2016, https://www.guttmacher.org/fact-sheet/induced-abortion-united-states#8.
- Lawrence B. Finer, Lori F. Frohwirth, Lindsay A. Dauphinee, Susheela Singh, and Ann M. Moore, “Reasons U.S. Women Have Abortions: Quantitative and Qualitative Perspectives,” Perspectives on Sexual and Reproductive Health, September 2005, Volume 37, Issue 3, p. 110–118, https://www.guttmacher.org/journals/psrh/2005/reasons-us-women-have-abortions-quantitative-and-qualitative-perspectives.
- “Roe v. Wade,” CaseLaw.FindLaw.com, http://caselaw.findlaw.com/us-supreme-court/410/113.html.
- “Planned Parenthood of Southeastern Pennsylvania v. Casey,” Legal Information Institute, https://www.law.cornell.edu/supremecourt/text/505/833#.
- Elizabeth Nash, Rachel Benson Gold, Zohra Ansari-Thomas, Olivia Cappello, Lizamarie Mohammed, “Laws Affecting Reproductive Health and Rights: State Trends at Midyear, 2016,” Guttmacher Institute, July 21, 2016, https://www.guttmacher.org/article/2016/07/laws-affecting-reproductive-health-and-rights-state-trends-midyear-2016.
- Elizabeth Nash et al, “Policy Trends in the States: 2016,” Guttmacher Institute, January 2017, https://www.guttmacher.org/article/2017/01/policy-trends-states-2016.
- Ibid.
- Alexa Ura, “Texas Case Could Define Extent of Abortion Limits,” Texas Tribune, February 28, 2016, https://www.texastribune.org/2016/02/28/abortion-rulings-texas/.
- Alexa Ura, “U.S. Supreme Court Overturns Texas Abortion Restrictions,” Texas Tribune, June 27, 2016, https://www.texastribune.org/2016/06/27/us-supreme-court-rules-texas-abortion-case/.
- “Whole Woman’s Health v. Hellerstedt,” SCOTUS Blog, 2016, http://www.scotusblog.com/case-files/cases/whole-womans-health-v-cole/.
- Erik Eckholm, “Oklahoma Governor Vetoes Bill That Would Charge Abortion Doctors,” New York Times, May 20, 2016, http://www.nytimes.com/2016/05/21/us/oklahoma-governor-mary-fallin-vetoes-abortion-bill.html?_r=0.
- “Oklahoma Senate Bill 1552,” Legiscan, 2016, https://legiscan.com/OK/bill/SB1552/2016.
- Erik Eckholm, “Oklahoma Governor Vetoes Bill That Would Charge Abortion Doctors,” New York Times, May 20, 2016, http://www.nytimes.com/2016/05/21/us/oklahoma-governor-mary-fallin-vetoes-abortion-bill.html?_r=0.
- Franciscan Alliance v. Burwell, Civil Action 7:16, U.S. District Court of Northern Texas (2016).
- Rachel K. Jones and Jenna Jerman, “Abortion Incidence and Service Availability in the United States, 2011,” Guttmacher Institute, 2014, https://www.guttmacher.org/sites/default/files/article_files/abortion_incidence_in_the_united_states_2011.pdf.
- Ibid.
- Ibid.
- “USA Counties,” U.S. Census Bureau, 2016, https://censtats.census.gov/usa/usainfo.shtml.
- Rachel K. Jones and Jenna Jerman, “Abortion Incidence and Service Availability in the United States, 2011,” Guttmacher Institute, 2014, https://www.guttmacher.org/sites/default/files/article_files/abortion_incidence_in_the_united_states_2011.pdf.
- “Publicly Funded Family Planning Services in the United States,” Guttmacher Institute, September 2016, https://www.guttmacher.org/fact-sheet/publicly-funded-family-planning-services-united-states.
- Jennifer Frost and Kinsey Hasstedt, “Quantifying Planned Parenthood’s Critical Role in Meeting the Need for Publicly Supported Contraceptive Care,” Health Affairs Blog, September 8, 2015, http://healthaffairs.org/blog/2015/09/08/quantifying-planned-parenthoods-critical-role-in-meeting-the-need-for-publicly-supported-contraceptive-care/.
- “Planned Parenthood Health Centers by State,” Planned Parenthood, 2016, https://www.plannedparenthood.org/about-us/local-state-offices/planned-parenthood-health-centers-by-state.
- “Annual Estimates of the Resident Population: April 1, 2010 to July 1, 2015: 2015 Population Estimates,” U.S. Census Bureau, May 2016, https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- “Find A Provider,” National Abortion Federation,” 2016, https://prochoice.org/think-youre-pregnant/find-a-provider/.
- While it can be approximated from TCF research and Guttmacher’s existent survey of nationwide abortion providers that there are roughly 200 more abortion clinics across the country (Rachel K. Jones and Jenna Jerman, “Abortion Incidence and Service Availability in the United States, 2011,” Guttmacher Institute, 2014, https://www.guttmacher.org/sites/default/files/article_files/abortion_incidence_in_the_united_states_2011.pdf.)—not including hospitals and physician’s offices that can provide abortions, but often don’t—beyond the Planned Parenthood centers and NAF members shown in the below map, they are extremely difficult to find. When using Google searches for clinics to obtain abortions other than Planned Parenthood clinics, users are yielded an array of pro-life articles (Bre Payton, “Fact Check: Yes, Women Can Go Elsewhere if Planned Parenthood Closes,” The Federalist, September 28, 2015, http://thefederalist.com/2015/09/28/fact-check-yes-women-can-go-elsewhere-if-planned-parenthood-closes/.) propagating women’s health groups that do not offer abortion services as a replacement for Planned Parenthood centers.
- Ford Fessenden, “How the Supreme Court’s Decision Will Affect Access to Abortion,” New York Times, June 27, 2016, http://www.nytimes.com/interactive/2016/02/29/us/why-the-abortion-clinics-have-closed.html?action=click&contentCollection=U.S.&module=RelatedCoverage®ion=Marginalia&pgtype=article.
- “An Overview of Abortion Laws,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/overview-abortion-laws.
- Ibid.
- “Is Abortion Linked to Breast Cancer?,” American Cancer Society, June 19, 2014, http://www.cancer.org/cancer/breastcancer/moreinformation/is-abortion-linked-to-breast-cancer.
- “An Overview of Abortion Laws,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/overview-abortion-laws.
- “Counseling and Waiting Periods for Abortion,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/counseling-and-waiting-periods-abortion.
- “Requirements for Ultrasound,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/requirements-ultrasound.
- “State Policies on Later Abortions,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/state-policies-later-abortions.
- Franklin Foer, “Fetal Viability,” Slate News, May 25, 1997, http://www.slate.com/articles/news_and_politics/the_gist/1997/05/fetal_viability.html.
- “An Overview of Abortion Laws,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/overview-abortion-laws.
- “Public Funding for Abortion,” ACLU, 2016, https://www.aclu.org/other/public-funding-abortion.
- Alina Salganicoff, Laurie Sobel, Nisha Kurani, and Ivette Gomez, “Coverage for Abortion Services in Medicaid, Marketplace Plans and Private Plans,” The Henry J. Kaiser Family Foundation, January 20, 2016, http://kff.org/womens-health-policy/issue-brief/coverage-for-abortion-services-in-medicaid-marketplace-plans-and-private-plans/.
- Ibid.
- “State Funding of Abortion Under Medicaid,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/state-funding-abortion-under-medicaid.
- Kinsey Hasstedt, “Abortion Coverage Under the Affordable Care Act: Advancing Transparency, Ensuring Choice and Facilitating Access,” Guttmacher Policy Review, Volume 18, Issue 1, April 9, 2015, https://www.guttmacher.org/gpr/2015/04/abortion-coverage-under-affordable-care-act-advancing-transparency-ensuring-choice-and.
- “Induced Abortion in the United States,” Guttmacher Institute, September 2016, https://www.guttmacher.org/fact-sheet/induced-abortion-united-states#8.
- Jenna Jerman, Rachel K. Jones, and Tsuyoshi Onda, “Characteristics of U.S. Abortion Patients in 2014 and Changes Since 2008,” Guttmacher Institute, May 2016, https://www.guttmacher.org/report/characteristics-us-abortion-patients-2014.
- “Title X Family Planning,” HHS.gov, https://www.hhs.gov/opa/title-x-family-planning/.
- Elizabeth Nash, Rachel Benson Gold, Zohra Ansari-Thomas, Olivia Cappello, Lizamarie Mohammed, “Laws Affecting Reproductive Health and Rights: State Trends at Midyear, 2016,” Guttmacher Institute, July 21, 2016, https://www.guttmacher.org/article/2016/07/laws-affecting-reproductive-health-and-rights-state-trends-midyear-2016.
- “Planned Parenthood at a Glance,” Planned Parenthood, 2016, https://www.plannedparenthood.org/about-us/who-we-are/planned-parenthood-at-a-glance.
- “Compliance With Title X Requirements by Project Recipients in Selecting Subrecipients,” Health and Human Services Department, Office of the Federal Register, September 7, 2016, https://www.federalregister.gov/documents/2016/09/07/2016-21359/compliance-with-title-x-requirements-by-project-recipients-in-selecting-subrecipients.
- Jackie Calmes, “Obama Bars States from Denying Federal Money to Planned Parenthood,” New York Times, December 14, 2016, http://www.nytimes.com/2016/12/14/us/politics/obama-administration-planned-parenthood.html.
- Ibid.
- “Statement: NARAL Pro-Choice America and NARAL Pro-Choice Massachusetts on Supreme Court Decision to Strike Down Buffer Zones in McCullen v. Coakley,” NARAL Pro-Choice America, June 26, 2014, http://www.prochoiceamerica.org/media/press-releases/2014/pr6262014_scotus_buffer_zone.html.
- Tracy A. Weitz et al, “Safety of Aspiration Abortion Performed by Nurse Practitioners, Certified Nurse Midwives, and Physician Assistants Under a California Legal Waver,” Am J Public Health, Volume 103, Issue 3, March 2013, p. 454–461, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3673521/.
- Olga Khazan, “Abortion Privilege Under Trump,” The Atlantic, November 17, 2016, http://www.theatlantic.com/health/archive/2016/11/trumps-traveling-plan-for-abortions/507947/.
- Joseph E. Potter, “Texas Policy Evaluation Project,” The University of Texas at Austin, 2016, http://liberalarts.utexas.edu/txpep/.
- Olga Khazan, “Texas Women Are Inducing their Own Abortions,” The Atlantic, November 17, 2016, http://www.theatlantic.com/health/archive/2015/11/texas-self-abort/416229/.
- “Planned Parenthood at a Glance,” Planned Parenthood, 2016, https://www.plannedparenthood.org/about-us/who-we-are/planned-parenthood-at-a-glance.
- “Birth Control Benefits,” Healthcare.gov, https://www.healthcare.gov/coverage/birth-control-benefits/.
- Robert Pear, “Tom Price, Obamacare Critic, Is Trump’s Pick for Health Secretary,” New York Times, November 28, 2016, http://www.nytimes.com/2016/11/28/us/politics/tom-price-secretary-health-and-human-services.html?_r=0.
- Claire Landsbaum, “In the Middle of the Night, the Senate Voted Against Keeping Health-Care Coverage for Contraceptives,” New York Magazine, January 12, 2017, http://nymag.com/thecut/2017/01/the-senate-just-voted-to-roll-back-womens-healthcare.html?mid=facebook_thecutblog.
- Elizabeth Nash, Rachel Benson Gold, Zohra Ansari-Thomas, Olivia Cappello, Lizamarie Mohammed, “Laws Affecting Reproductive Health and Rights: State Trends at Midyear, 2016,” Guttmacher Institute, July 21, 2016, https://www.guttmacher.org/article/2016/07/laws-affecting-reproductive-health-and-rights-state-trends-midyear-2016.
- Pamela Wood, “New Law Puts Marylands at ‘Forefront’ of Birth Control Access,” Baltimore Sun, May 9, 2016, http://www.baltimoresun.com/news/maryland/politics/bs-md-birth-control-copay-20160509-story.html.
- Elizabeth Nash, Rachel Benson Gold, Zohra Ansari-Thomas, Olivia Cappello, Lizamarie Mohammed, “Laws Affecting Reproductive Health and Rights: State Trends at Midyear, 2016,” Guttmacher Institute, July 21, 2016, https://www.guttmacher.org/article/2016/07/laws-affecting-reproductive-health-and-rights-state-trends-midyear-2016.
- Jessica Firger, “Birth Control Pill Is Now Available in Oregon and California Without a Prescription,” Newsweek, January 4, 2016, http://www.newsweek.com/birth-control-pill-now-available-oregon-and-california-without-prescription-411357.
- Zack Hale, “Planned Parenthood Hails Hawaii Birth Control Law,” State of Reform, July 8, 2016, http://stateofreform.com/featured/2016/07/planned-parenthood-hails-hawaii-birth-control-law/.
- “Abortion Policy in the Absence of Roe,” Guttmacher Institute, December 1, 2016, https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe.
- The Editorial Board, “Protecting Reproductive Rights Under Donald Trump,” New York Times, December 7, 2016, http://www.nytimes.com/2016/12/07/opinion/protecting-reproductive-rights-under-donald-trump.html?action=click&pgtype=Homepage&clickSource=story-heading&module=opinion-c-col-left-region®ion=opinion-c-col-left-region&WT.nav=opinion-c-col-left-region&_r=0.
- Pamela Wood, “New Law Puts Marylands at ‘Forefront’ of Birth Control Access,” Baltimore Sun, May 9, 2016, http://www.baltimoresun.com/news/maryland/politics/bs-md-birth-control-copay-20160509-story.html.
- Alex Zielinski, “Maryland Passes the Most Sweeping Birth Control Access Law in the Country,” Think Progress, May 11, 2016, https://thinkprogress.org/maryland-passes-the-most-sweeping-birth-control-access-law-in-the-country-2fe6dbfb1f40#.di1lx8s53.
- “Fact Sheet: State of Contraceptive Coverage in the United States,” NARAL Pro-Choice America, November 16, 2016, http://www.prochoiceamerica.org/media/press-releases/2016/pr11162016_fact_sheet_contraceptive_coverage_trump.html.
- “Reproductive Rights Emerge from 2015 Montana Legislature Stronger Than Ever,” NARAL Pro-Choice America, May 15, 2015, http://www.prochoicemontana.org/news/press/20150515.shtml.
- “Planned Parenthood, ACLU, and Center for Reproductive Rights File Simultaneous Challenges to Abortion Restrictions in Three States,” Planned Parenthood, November 30, 2016, https://www.plannedparenthood.org/about-us/newsroom/press-releases/planned-parenthood-aclu-and-center-for-reproductive-rights-file-simultaneous-challenges-to-abortion-restrictions-in-three-states.
- Ibid.
- “Healthcare Providers Challenge Arizona Law Designed to Exclude Abortion Providers from State’s Medicaid Program,” ACLU, July 14, 2016, https://www.aclu.org/news/healthcare-providers-challenge-arizona-law-designed-exclude-abortion-providers-states-medicaid.
- “Federal Judge Blocks Two Alabama Abortion Restrictions,” ACLU, October 28, 2016, https://www.aclu.org/news/federal-judge-blocks-two-alabama-abortion-restrictions.
- “Women’s March on Washington,” www.womensmarch.com, 2017, https://www.womensmarch.com.
- “Volunteer and Internship Opportunities,” Planned Parenthood, 2017, https://plannedparenthoodrccorpvolunteer.peoplefluent.com/joblist.html?erpc=alljobs.
- Hannah Fingerhut, “About Seven-in-Ten Americans Oppose Overturning Roe v. Wade,” Pew Research Center, January 3, 2017, http://www.pewresearch.org/fact-tank/2017/01/03/about-seven-in-ten-americans-oppose-overturning-roe-v-wade/.
- Ibid.










