The United States is facing a massive worker safety crisis. As the COVID-19 pandemic grew in strength, and many workplaces moved to remote work or shut down entirely to avoid the contagion, millions of workers risked their lives by continuing to go into work to care for the nation’s sick and elderly, to help families put food on their tables, to get people to and from work, and ensure public safely. The toll on these essential workers—and on their families and communities—has been enormous. The Centers for Medicare and Medicaid Services (CMS), reported as of September 6, 2020, almost 300,000 confirmed or suspected COVID-19 infections among nursing home staff, of whom 868 have been killed by the disease.1 Thousands more health care personnel in hospitals have also been sickened; however there is no comprehensive, accurate count of these numbers.2
As the pandemic has continued, tens of thousands of other workers—emergency responders, corrections officers, transit workers, meat and poultry processing workers, farm workers, grocery store and warehouse workers, and many others—have been sickened and hundreds more of them have died.
COVID-19 has had a disproportionate and tragic impact on communities of color: working-age African Americans and Latinx people are at greatly increased risk of the COVID-19 disease and death.3 Much of this increase is driven by employment patterns: racial and ethnic minorities are overrepresented in the essential and frontline jobs that cannot be done by teleworking from home. The jobs held by these workers put them in close contact with other workers and the public, and they are often given inadequate respirators or other personal protective equipment (PPE). Many of these workers travel to and from work in crowded public or semi-private transportation. Since the virus does not stop at the door of the factory or nursing home or prison or subway car, these workers bring the pandemic into their homes and communities.
Even though COVID-19 continues to spread, with tens of thousands of new cases reported each day and over 200,000 deaths so far, across the country businesses are re-opening. The many workers who never have had the opportunity to protect themselves by working remotely are now being joined by others newly returning to worksites—many of them now exposed to potentially dangerous conditions. All these workers need to be protected. If workplace exposures are not controlled, more workers—along with members of their families and communities—will be infected, causing more illness and death, and threatening the ability of the nation to resume economic growth.
This report looks briefly at the conditions under which COVID-19 has continued to spread through workplace transmission and assesses the failures of OSHA and the federal government to protect workers from exposure. It then presents an eleven-point plan—to be directed by the federal government, working in close coordination with state and local public health authorities—for stopping workplace transmission of COVID-19.
Work Exposures and the Spread of the Virus
To understand the central role of workplace exposures in driving the spread of the virus, consider nursing homes and long-term care facilities, where COVID-19 has had catastrophic effects on both residents and workers. Conditions in these understaffed facilities promote the rapid spread of the virus.4 Nursing homes were slow to adopt effective infection control procedures and workers in many nursing homes still have, at best, limited access to essential PPE such as respirators and gowns. Hundreds of nursing homes have not secured or have run out of N95 respirators (that protect the wearer from infection) and many are reported to be near the end of their supply of protective gowns and surgical masks (that primarily protect others in case the wearer is infected).5 Many low-paid nursing home workers hold jobs in more than one facility in order to earn enough to support their families. It is inevitable that these inadequately protected workers, going from facility to facility, contract the virus and bring it into their homes and communities and help spread the pandemic to other workplaces.

Farms and processing facilities along the food supply chain play a similar role in spreading the virus. Migrant farmworkers are often provided substandard housing with many beds in the same room and are typically driven to the fields in crowded vans and buses. It is difficult to know how many farm workers have been infected by the virus, since there is so little testing done on these underpaid, often migrant workers. Purdue University estimates the number is greater than 125,000.6
Even before the COVID-19 pandemic, workers in meat and poultry plants were at high risk of occupational injury and illness. These workers do their jobs in very tight conditions, elbow to elbow, cutting pieces of pork or beef or chicken that move rapidly past them on assembly lines. The buildings are like giant refrigerators—kept cold to reduce spoilage, with little fresh air flow—an environment conducive to virus spread. Workers report the processing lines run so fast that they do not have time to cover their face with their arms when they sneeze or cough.

The efforts to combat virus transmission at food processing plants have been dangerously inadequate. Meat companies responsible for bulk of meat production have failed to implement many of the safe work practices recommended by the CDC and OSHA for protecting workers from virus exposure.7 And although CDC has investigated COVID-19 outbreaks at a few of the meat factories, the federal government has made only limited efforts to count the total number of infected workers.8 By late September, the Food and Environment Reporting Network had compiled reports from local health departments that total 44,000 infected meat workers, including more than 200 deaths.9
Map 1. COVID-19 Outbreaks in the Food System
Source: Map courtesy of Leah Douglas of the Food and Environment Reporting Network, https://thefern.org/2020/04/mapping-covid-19-in-meat-and-food-processing-plants/.
Increased risk of disease or death faces workers in any situation where they have extensive unprotected exposures to other workers, the public, or other persons who may be infectious. Prisons, jails, and immigrant detention centers have all been the sites of large outbreaks of COVID-19 and many staff in these facilities have been sickened. Similarly, cities across the country report numerous infections and deaths among bus drivers and other public transportation workers.10 Temporary workers, sent by staffing agencies into short-term work assignments, are at especially high risk, since they are often not provided adequate PPE or the ability to distance, and, because of their employment status, have little ability to even request safer conditions.11
There is little question that structural racism contributes to the nation’s failure to address worker exposures occurring in these industries.12 While people of color, many of whom are immigrants, are over-represented among the “essential” workers at greatest risk for disease and death,13 their safety appears to be of little concern to some white civic leaders. For example, in discussing an outbreak of almost 800 COVID-19 cases in Brown County, where many of the meat workers are immigrants, the Chief Justice of the Wisconsin Supreme Court dismissed any concern, noting “These were due to the meatpacking. . . . It wasn’t just the regular folks in Brown County.” Similarly, when the pork producer Smithfield Foods had to temporarily stop production at its Sioux Falls, South Dakota plant after more than 1,000 workers were infected, South Dakota Governor Kristi Noem blamed the problem on the workers’ home lives, baselessly asserting “99% of what’s going on today wasn’t happening inside the facility.”14
Even before COVID-19, much of the impact of workplace injury and illness fell on low-wage workers.15 As a result, work injuries and illnesses contribute to the growth in the nation’s economic inequality; injuries and illnesses block low-wage workers from entering the middle class and throw better-paid workers into poverty.16 The failure of the workers’ compensation system to provide adequate benefits for these workers forces many of them into taxpayer-supported programs such as Social Security Disability Insurance. COVID-19 has highlighted the inadequacies of the workers’ compensation system and the disparities between states in terms of coverage and benefits for work-related diseases. As the pandemic continues to course through U.S. workplaces, it will only accelerate these trends, absent serious regulatory intervention.

The impact of workplace transmission is evident in the geography of the pandemic. Across the country, many of the counties who have had the highest COVID-19 rates and fastest growth rates are those with prisons or meat production plants, large facilities with many people in close proximity with no ability to socially distance and who are provided inadequate or no PPE. 17Outbreaks in farms and food production facilities have seeded the virus in rural counties in every part of the country.
OSHA and the Failure of the Federal Response
Seven months into the COVID-19 pandemic, the federal government still lacks a comprehensive plan to control workplace virus exposure. As more businesses across the nation reopen, this failure will lead to increased workplace transmission of the virus and its inevitable spread to workers’ homes and communities, setting back efforts to save lives, stem the pandemic, and rebuild the nation’s economy.
With COVID-19, the Occupational Safety and Health Administration (OSHA) is facing the most significant challenge in its history. The agency’s mission is to assure protection of the safety and health of the nation’s workers, and it should be leading the federal government’s effort to stop workplace transmission of the virus. OSHA has never been more in the headlines; unfortunately, this national attention is more because of its failures than its successes in addressing the COVID-19 worker safety crisis.18
OSHA has never been more in the headlines; unfortunately, this national attention is more because of its failures than its successes in addressing the COVID-19 worker safety crisis.
Under the Occupational Safety and Health Act of 1970 (the OSHAct), employers are required to provide workplaces free from recognized serious hazards.19 In other words, every worker has the right to a safe workplace, and OSHA’s job is to protect this right by ensuring that employers eliminate hazards that could injure or sicken workers. Stemming this pandemic will require employers to restructure and reorganize work settings to minimize transmission. OSHA should be making a substantial contribution to this effort nationally, but it has chosen to play a minor, advisory role providing safety tips and soft recommendations (see below), but rarely requiring employers to provide adequate protection for their employees.
Years of research, investigation, and OSHA enforcement efforts during disease outbreaks associated with influenza, corona viruses, and other airborne pathogens have taught us a great deal about how to prevent workplace transmission of COVID-19. It is clear that, until there is an effective vaccine or we can be confident that people who are shedding virus are completely stopped from entering workplaces, it is necessary to apply a series of preventive measures, no single one of which is adequate by itself. These measures include screening, isolation or quarantine of infected/likely infected/close-contact workers, enhanced ventilation, physical distancing, respiratory and other personal protective equipment (PPE), sanitation, and disinfection.
Employers are more likely to implement these controls if they are required by a government agency that has the enforcement tools to compel those actions. The success of OSHA’s bloodborne pathogens (BBP) standard is an example of this approach. The standard was issued in response to the HIV/AIDS crisis of the 1980s and 1990s; it requires health care employers to develop an infection control plan, properly dispose of needles and other sharp instruments, and provide free Hepatitis B vaccinations. The BBP standard has contributed to a dramatic drop in health care worker risk for HIV and Hepatitis B and C and played an important role in the nation’s successful response to its 2014 Ebola outbreak.
OSHA is primarily an enforcement agency that issues standards and inspects workplaces and issues citations resulting from violations of its standards. The hundreds of standards that OSHA enforces cover hazards ranging from fall protection to toxic chemicals to bloodborne pathogens. Although OSHA began work on a standard covering infectious diseases in response to the H1N1 pandemic of 2009, that effort was ended by the Trump administration and has not been resurrected.20
It can take OSHA anywhere between ten and twenty years to issue a major standard, but the Occupational Safety and Health Act also contains a provision authorizing OSHA to issue an Emergency Temporary Standard (ETS) for new hazards that pose a “grave danger” to workers. Secretary of Labor Eugene Scalia and the Trump administration have made the decision that neither OSHA nor the Mine Safety and Health Administration (MSHA), the agency with similar responsibilities to issue and enforce health and safety standards for US miners, would issue Emergency Temporary Standards requiring employers to provide safe work environments for workers exposed to SARS-CoV-2. Instead, they are asking employers to follow voluntary guidance and recommendations issued by OSHA, MSHA, and the CDC. While these recommendations are useful in helping those employers who are willing to make the efforts necessary to control virus spread in their establishments, there are many employers who are not willing to do this. Recommendations from these agencies are not legally binding and, as witnessed in all too many worksites—from warehouses to meatpacking to fast food restaurants—enforceable rules are necessary when dealing with the large numbers of employers who need clear forceful rules to be motivated to take the actions required to make their workplaces safe.
The Occupational Safety and Health Act also contains a provision authorizing OSHA to issue an Emergency Temporary Standard (ETS) for new hazards that pose a “grave danger” to workers.
In the absence of mandatory federal standards, many states and localities have issued their own requirements, often under their emergency authorities; however, in the absence of a federally approved state OSHA plan, their authorities and relevant enforcement experience cannot match that of federal OSHA. While this patchwork of measures is better than nothing, the variation in requirements from locality to locality leaves many workers unprotected and makes it difficult for employers to know what measures are needed to protect workers from COVID-19.
Further, the recommendations currently issued by OSHA and CDC are generally soft pedaled, asking employers to “consider” providing life-saving precautions such as social distancing, “if feasible,” leaving it up to the employer to decide if making life-saving investments in worker safety is feasible. Consider this advice from the agencies’ recommendations to meat and poultry processing workers and employers:
Modify the alignment of workstations, including along processing lines, if feasible, so that workers are at least six feet apart in all directions (e.g., side-to-side and when facing one another), when possible. (italics added). 21
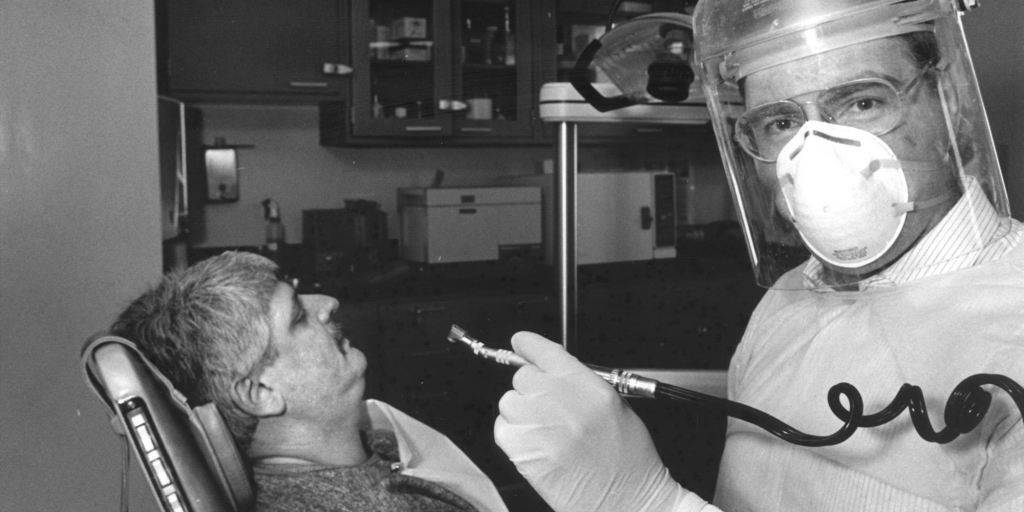
Or consider an example of OSHA advice sent to all employers on OSHA’s email mailing list (see Figure 1).
Figure 1. OSHA Advice on Wearing Masks
Imagine if, using the same photo, the objective of this mass communication was to increase the use of hard hats on construction sites. In that case, the text of the message would have read “OSHA regulations state that employers must require workers to wear hard hats to protect their heads from falling objects.” Every employer knows that failure to insist their employees wear hard hats can result in an OSHA fine (as well as an injured worker), so bare-headed workers are rarely seen at construction sites. But OSHA is unwilling to make the same requirement around masks, physical distancing, ventilation, or most other COVID-related safety precautions.
OSHA: Potentially Effective, but Under-Resourced and Underused
This year is the fiftieth anniversary of the passage of the OSHAct, the legislation that launched OSHA and its sister agency, the National Institute for Occupational Safety and Health (NIOSH). There is little question that OSHA’s past efforts have saved tens of thousands of lives and prevented millions of injuries. In the first year of OSHA’s existence, thirty-seven workers nationwide were killed on the job every day; now, with a workforce more than twice as large, that figure has dropped to fourteen deaths from traumatic injuries each day. Until recently, there had also been a significant drop in rates of non-fatal workplace injuries.22 There is extensive evidence that OSHA standards are effective in preventing injuries and illnesses, and that OSHA inspections lead to decreases in injuries for several years after a workplace is inspected.23
While overall OSHA has been successful in reducing the toll of work injury and illness, it is often misunderstood and sometimes ridiculed by politicians and others who don’t believe the government should be telling businesses how to operate—even if those requirements are meant to prevent lethal injury or fatal illness among its workers. One recent example: in asserting his opposition to proposed legislation strengthening OSHA’s response to COVID-19, Senator John Kennedy (R-LA) attempted to ridicule the agency: “I don’t want to have to wear a face mask in the shower. That’s the sort of stuff that OSHA promulgates every day.”24
Historically, OSHA has been faced with an immense challenge and has never been able to fulfill its mission adequately. Despite OSHA’s past successes, more than 5,000 workers are still killed on the job every year, and the fatal injury rate remains stubbornly high. Currently, employers report more than 3 million workers are injured on the job each year, and, according to the Bureau of Labor Statistics, this is a significant undercount of the actual number of injuries.25 The rates of fatal and non-fatal injuries are no longer declining, and changes in the workplace and the workforce have made OSHA’s tools and approaches less effective in growing sectors of the economy, such as health care and warehousing, for which OSHA has far fewer standards applicable to specific hazards in these industries. Furthermore, OSHA has not compiled any reasonably accurate estimates of the number of work-related illnesses that occur each year, even though it is estimated that almost 100,000 U.S. workers die annually from past exposures to toxic substances alone.26
OSHA is staffed with highly competent, committed safety and health professionals. However, this small agency is severely under-resourced, given the enormity and importance of its mission, even without the added challenges caused by the pandemic. OSHA’s annual budget is less than $600 million—a fraction of the $8 billion Environmental Protection Agency budget, for example. OSHA covers between seven and eight million workplaces, where more than 130 million workers are employed. The federal agency, together with the State OSHA plans, have around 2,000 inspectors; in 1980, the agency had 14.8 inspectors for every million covered workers; by 2018, that ratio had dropped to 5.6. OSHA today has the smallest number of inspectors in the past forty years.27 With current staffing, it would take federal OSHA 165 years to visit every establishment in its jurisdiction one time.
OSHA’s annual budget is less than $600 million—a fraction of the $8 billion Environmental Protection Agency budget, for example.
Many OSHA staff and career leadership would like to do much more to increase protections for COVID-19 exposed workers but are frustrated by the agency’s inaction. However, as the pandemic exploded first in health care facilities then in other industries across the country infecting many thousands of workers, OSHA has kept a low profile. It has opened very few actual inspections and issued just a handful of citations.
OSHA’s Pandemic Response: Absence and Inaction
As the pandemic began to spread, workers at meat packing plants across the country sent complaints to OSHA, reporting crowded production lines and break rooms—at a time when everyone in the country was being cautioned repeatedly to keep six feet apart. When hundreds of meat processing workers at Smithfield, Tyson, JBS, and other multinational corporations were found to be infected, the Trump administration made little effort to insist that the firms implement protective measures.28 With a handful of exceptions, OSHA’s response to worker complaints was not to launch an inspection; it simply sent letters to the employers asking for more information about exposure, and then closed the cases.
A strong message from the administration focused on worker safety might have prevented thousands of infections and scores of deaths. Instead, the Trump administration launched an effort to help the meat processing industry maintain operations no matter the human toll. At the request of the meat industry, President Trump issued an Executive Order,29 much of which was written by the industry, that was used to intimidate local public health authorities and keep meat factories open even when large numbers of workers were being sickened and killed by the virus.30
OSHA’s failure to use enforcement to motivate more employers to protect workers from COVID-19 is exemplified by the results of its inspections at two meat factories. Many months after workers at the Smithfield Foods pork plant in Sioux Falls, South Dakota first complained about conditions that were causing runaway COVID-19 infections, OSHA finally completed its inspection in September. OSHA found the firm failed to implement social distancing as a protective measure, resulting in the infection of almost 1,300 workers, four of whom were killed and forty-three of whom had to be hospitalized. The punishment? OSHA fined Smithfield $13,494, for a single serious violation, disingenuously claiming it was “the maximum fine allowed by law.”31
After at least 290 workers at the JBS beef factory in Greeley, Colorado were infected and six were killed by the virus, OSHA fined the firm $15,615.
Similarly, after at least 290 workers at the JBS beef factory in Greeley, Colorado were infected and six were killed by the virus, OSHA fined the firm $15,615: $13,494 for a single serious violation, and an additional $2,121 for not providing the union access to the log in which JBS tracked worker illnesses. Again, OSHA claimed that the fine for the single serious violation was “the maximum allowed by law.”32 The Greeley Tribune calculated that, since JBS’s net revenue in 2019 was $51.7 billion in 2019, the fine represented 0.00003 percent of last year’s profits: “the equivalent of fining someone making $50,000 a year—an approximate salary for a meat cutter at the Greeley plant,—one-and-a-half cents.”33 The family of one of the workers who died reported that the cost of the funeral was more than the OSHA fine.34
President Donald Trump’s appointees at the Department of Labor clearly made the decision to go easy on Smithfield and JBS. While a $13,494 penalty is “the maximum fine allowed by law” for a single serious violation, OSHA could have issued numerous citations for the various departments where Smithfield and JBS failed to protect workers, and it could have designated them as willful violations, with penalties ten times greater than the ones imposed. In 2005, for example, OSHA issued $21,361,500 in penalties to BP after an explosion that killed fifteen workers. BP received an $81 million fine four years later for failure to abate the hazards cited in the first citation.35
Even with these minimal fines, these two multi-billion dollar global corporations (JBS is Brazilian-owned, and Smithfield is Chinese) have announced they will contest the citations and fines. This allows them to save face as well as to avoid having to abate the hazards that OSHA identified, since the law allows employers to wait until the case is completely resolved before they have to address the hazards for which they were cited. On behalf of JBS and Smithfield, their trade association, the North American Meat Institute, issued a press release attacking the OSHA citations as “confusing and revisionist,” claiming the firms were in fact following those weak CDC/OSHA recommendations. After all, the meat companies wrote that “CDC/OSHA guidance acknowledged being six feet apart is not always possible” and “OSHA states that companies that adhere to the Guidance need not fear citation.”36
Every OSHA enforcement action sends a message. Since an important objective of enforcement actions is to remind other employers that failure to protect workers has consequences, the decision to issue minimal fines on JBS and Smithfield has enormous implications for COVID-19 exposed workers across the country. Through OSHA’s actions, Labor Secretary Eugene Scalia is sending the clear message to employers that they need not worry about OSHA inspections—they can operate as they please, permitting uncontrolled exposure to the deadly virus, since the firms have no reason to fear a costly OSHA penalty no matter how many workers are sickened or killed.
The Department of Agriculture has given poultry processing plants, many of which are the sites of large outbreaks of COVID-19, permission to speed up production lines during the pandemic.
There is also notable lack of coordination across federal agencies, and several have refused to take actions that would reduce exposure. The Department of Agriculture has given poultry processing plants, many of which are the sites of large outbreaks of COVID-19, permission to speed up production lines during the pandemic,37 which will likely increase already high transmission risk. The Department of Transportation has refused to issue rules requiring passengers and flight attendants to wear face masks, with Transportation Secretary Elaine Chou declaring that mask wearing is a “labor-management issue.”38
The Trump administration’s unwillingness to address workplace exposure is just one component of the incompetent, uncaring, and consequently tragic overall response of the federal government to the pandemic. Instead of mounting a coordinated public health effort, we now have only a patchwork of responses and policies.
There are also efforts to substantially constrain OSHA in the future, were it to start embracing a more active role in worker protection during the pandemic. Legislation proposed by Senator Mitch McConnell (R-KY) and the Senate Republican leadership to limit employer liability from COVID-related lawsuits is a significant threat to the ability of the federal and state governments to use their authorities to compel employers to provide safe workplaces. In addition to making lawsuits by infected workers or the families of deceased workers far more difficult and unlikely to succeed, a lesser known provision of the law would exempt an employer from any federal or state inspection or enforcement action if they made the most minimal effort to consider protecting workers. If this law were to be enacted, employers could avoid having to meet the requirements of any labor law if they are able to show simply that they were “exploring options to comply with such obligations and with the applicable government standards and guidance”—not that they had to meet any existing OSHA standards or the already toothless recommendations.39
Recommendations for a Better Way Forward
A comprehensive plan, directed by the federal government, with federal agencies working in close coordination with state and local public health authorities, is badly needed. For the overall U.S. response to the pandemic to succeed, the federal government needs to take leadership in a concerted campaign aimed at stopping workplace transmission of COVID-19.
The following are components of this campaign that could be implemented immediately, for the most part without additional resources or Congressional authorization.
1. Elevate Worker Protection to the White House and Develop a National COVID-19 Worker Protection Plan
The nation must focus on enabling workers to work safely, since protecting workers is at the core of both controlling the pandemic and reopening the economy. This requires resolute national leadership, starting in the Oval Office, and a concerted effort to engage the public in this initiative. To launch this, the president should appoint a worker protection coordinator, based at the White House, to develop a comprehensive plan to actively engage the nation in this effort to protect workers, with OSHA stepping firmly into a prominent national leadership role. Businesses and unions are eager to participate and have been waiting for federal leadership to help them operate safely. The worker protection coordinator would also chair a Worker Protection Council, bringing together federal agencies with authority over different components of the economy.
In its initial plan to reopen the economy “Opening Up America Again,” the Trump administration assigned worker protection to the states, essentially abdicating OSHA’s role as the nation’s leader in workplace safety and health.40 It appears that the White House authors of this plan were not even aware that the twenty-nine states in which federal OSHA has responsibility for private sector workers have virtually no inspection or enforcement infrastructure of their own—and yet were being told to protect workers in the face of this massive workplace safety crisis.
In its initial plan to reopen the economy “Opening Up America Again,” the Trump administration assigned worker protection to the states, essentially abdicating OSHA’s role as the nation’s leader in workplace safety and health
The White House, through the worker protection coordinator and Worker Protection Council, should create a comprehensive roadmap that focuses on making workplaces safe, outlining the roles of federal agencies, state and local governments, employers and trade associations, unions and worker centers, public health and professional organizations, and other stakeholders, including the American Industrial Hygiene Association and the National Safety Council, who can assist employers in reducing COVID-19 exposure in their establishments.
Most important, the White House needs to educate and engage the country in recognizing the centrality of worker protection in efforts to control the virus. The coordinator should promptly convene a series of high-profile online meetings involving all of the groups listed above. The meetings and accompanying publicity would also serve to notify the country that the federal government is now actively leading efforts to keep workers and workplaces safe, and that doing so will require a concerted national effort.
In addition, through the Worker Protection Council, the coordinator should launch a series of multi-agency collaborative initiatives focusing on specific industries over which other agencies have significant leverage. In the past, for example, during the Obama administration, OSHA worked closely with the Federal Communications Commission to bring together the firms involved in cell tower construction and maintenance, insisting they collaborate to prevent tower climber fatalities.41 These new initiatives should include, at minimum:
- OSHA, the Centers for Medicare and Medicaid Services (CMS), and NIOSH should together engage the nursing home and assisted living and home care industries to better prevent COVID-19 exposure among their workers, an effort that will also reduce transmission to residents of these facilities and keep home care clients safe.
- Instead of asserting that the U.S. Department of Agriculture (USDA) has no role in worker safety, the USDA should work with OSHA to require meat and poultry firms to make those operations safer, insisting on slower, safer production lines, and only permitting faster lines if workers are adequately protected.
- The Department of Transportation should issue emergency rules requiring mask wearing on airplanes, passenger trains, interstate buses, and other modes of mass transportation under its jurisdiction.
- The Departments of Justice and Homeland Security should greatly enhance prevention efforts in the correctional and immigrant detention facilities they control.
- All new federal contracts should include provisions mandating that contractors implement effective Infection Control Plans.
Finally, in order to better target workplace interventions, much more needs to be known about the risk of infection in different industries, especially as more workplaces reopen. We know far more details about outbreaks in Major League Baseball teams than about the many COVID-19 outbreaks in meat factories, farms, jails, or mines. Some useful information will come from aggregating employer reports of COVID-19 cases, but a more comprehensive purposeful national data collection effort is necessary. The White House should direct and fund CDC (and specifically NIOSH, its work-focused component) to work closely with states to collect accurate and complete information about the employer and industry of all COVID-19 cases among working-age adults, and compile and report these data as promptly as possible. This will likely also require supplementing the funds provided to state and local health departments to gather and code information about COVID-19 cases.
- The White House should direct and fund CDC (and specifically NIOSH, its work-focused component) to work closely with states to collect accurate and complete information about the employer and industry of all COVID-19 cases among working-age adults, and compile and report these data as promptly as possible. This will likely also require supplementing the funds provided to state and local health departments to gather and code information about COVID-19 cases.
2. Require All Employers to Develop and Implement Infection Control Plans
The single most important action the Department of Labor can take to help stop this pandemic, save lives, and safely reopen the economy is for OSHA to issue an Emergency Temporary Standard (ETS), requiring all employers to develop and implement workplace infection control plans to prevent on-the-job COVID-19 transmission.42 Enforceable standards are OSHA’s most powerful and effective tool for protecting workers. Most employers are law-abiding and try to meet requirements issued by government agencies even before inspectors knock on the door. OSHA’s standards have prevented thousands of injuries and illnesses in industries in all parts of the economy.
Usually, OSHA standards take many years—even decades—to finalize.43 Following the H1N1 epidemic in 2009, OSHA began work on a standard that would have required hospitals, nursing homes, and other health care employers to develop and implement infection control plans, but this effort was ended by the Trump administration soon after taking office in early 2017.44
However, under the OSH Act, OSHA has the authority to quickly issue an ETS requiring employers to take immediate steps to prevent workers from COVID-19 exposure.45 Using this authority, OSHA should immediately issue an ETS requiring all employers under its jurisdiction46 to make and implement a comprehensive plan to control workplace exposures to the virus. The ETS would require employers to apply the hierarchy of controls,47 the widely accepted basic principles of industrial hygiene. This would include appropriate engineering controls, ventilation, physical distancing, PPE, sanitation, and disinfection and would require employers to meet, at minimum, all CDC and OSHA standards and recommendations (minus the modifications that suggest employers should “consider” precautions “if feasible”). MSHA should issue a similar ETS, tailored to the mines under its jurisdiction.
OSHA should immediately issue an ETS requiring all employers under its jurisdiction to make and implement a comprehensive plan to control workplace exposures to the virus.
OSHA’s general duty clause, the primary tool it is using now in the absence of an airborne infectious disease standard, is difficult to apply and does not provide clear direction for employers—it only tells employers to “keep your workplace safe.” Labor Secretary Scalia has refused to issue an ETS, falsely arguing that OSHA already has all the tools it needs to enforce safe working conditions.48 The AFL–CIO petitioned the Department of Labor for an ETS,49 but the request was rejected by Secretary Scalia.50
In order to assist employers in health care, meat packing, farming, and other high-risk industries, OSHA, in some cases jointly with CDC, has issued a series of voluntary recommendations, outlining the necessary steps employers should take to protect workers from on-the-job exposure to this deadly virus.51 But recommendations are far less effective than standards. Employers understand that they are not required to follow OSHA or CDC recommendations, but most will attempt to meet the requirements of clear, legally-enforceable standards. Like all of its guidance products, OSHA’s Guidance on Returning to Work begins with the advisory statement:
This guidance is not a standard or regulation, and it creates no new legal obligations. It contains recommendations as well as descriptions of mandatory safety and health standards. The recommendations are advisory in nature, informational in content, and are intended to assist employers in providing a safe and healthful workplace.52
OSHA’s statement makes it all too clear that employers are permitted to decide which is more important to them: production goals or the safety and health of their employees.
In contrast, mandatory standards are the traditional (and effective) way the government asserts that employers do not get to make this choice: workers must be protected. While the recommendations issued by OSHA and CDC can be useful (especially if the modifiers like “if feasible” discussed above are ignored), the tens of thousands of sick workers in health care facilities and meat factories are powerful proof that recommendations alone are not adequately effective in changing employer behavior.
Many workplaces, particularly meat and poultry factories, fail to come close to meeting these basic, life-saving requirements. There is extensive evidence that many asymptomatic individuals with SARS-CoV-2 infection carry significant viral loads and can spread the virus to others with whom they are in contact.53 Notwithstanding current CDC guidance allowing continued work by “close-contact” employees in essential industries (one of the politically driven recommendations coming from that beleaguered agency), employers must be required to pay workers who have been in close contact with infected coworkers to quarantine until it is known if they are infected—treating them the same way as CDC recommends that if they have been exposed to an infected friend or household member. The infection control plan required by the standard would be a type of safety and health management system (SHMS) program widely used by employers. OSHA has issued a SHMS guidance document that is a roadmap for successful hazard prevention.54
The HEROES Act, the pandemic relief bill passed by the House of Representatives last May, includes HR 6559, the COVID-19 Every Worker Protection Act of 2020.55 This bill would compel OSHA to issue an ETS, requiring employers to implement infectious disease exposure control plans based on CDC guidance. It would prohibit retaliation against workers who raise safety concerns (see below). Since the Department of Labor continues to refuse to issue this badly needed regulation, Congress should pass this legislation promptly.
3. Expedite Workplace Case Reporting and Response
Earlier in the pandemic, as large numbers of COVID-19 cases were first being reported in workplaces across the country, OSHA told all employers, other than those in the health care sector, that they did not have to record COVID-19 cases among their employees as work-related, which translates to telling employers there was no requirement to investigate if the infection could have been the result of an on the job exposure.56 After much criticism, OSHA reversed this directive, and employers now are required to record cases and therefore should attempt to determine if cases are work-related.57 Now, if a worker is hospitalized for COVID-19, the employer must report that to OSHA within twenty-four hours.
In order to control workplace transmission, OSHA needs to know where work-related outbreaks are occurring. One important tool for obtaining this information is a regulation requiring employers to report fatalities, hospitalizations, and amputations to OSHA. 58 Accordingly, earlier in the pandemic, OSHA reminded employers they were required to report hospitalizations of workers with COVID-19,59 and the first of the few citations that OSHA has issued for COVID-19 was for failure to report multiple hospitalizations that occurred among workers at a nursing home in Georgia. In early October, the Department of Labor suddenly withdrew this citation and announced a dramatic reinterpretation of the regulation.60 OSHA has instructed employers that they must report worker hospitalizations for COVID-19 only if they occur within twenty-four hours of their workplace exposure to the virus instead of twenty-four hours after the employer learns of the hospitalization.
Reporting hospitalizations within twenty-four hours of a workplace incident is appropriate for traumatic injuries such as falling off a roof, but it is nearly impossible to identify the precise moment of any single exposure incident involving COVID-19. Hospitalizations for COVID-19 often occur several days or longer after a person becomes infected, and infection occurs several days or weeks after an exposure incident. OSHA should immediately reverse this interpretation, since as it stands, very few COVID-related hospitalizations will be reported to OSHA in the future.
Workplaces where COVID-19 cases are clustered are likely ones where transmission is occurring. These are workplaces where immediate intervention may result in prevention of future cases. Employers are often among the first to learn when workers get sick. One case at a workplace might be from home or community transmission, but multiple cases suggest that exposures are occurring at work and should be investigated.61
Failure to identify work-related case clusters can delay important steps to reduce future cases.
Failure to identify work-related case clusters can delay important steps to reduce future cases. This is exactly what occurred, for example, in Worcester, Massachusetts, where there have been at least eighty-five cases and two deaths among workers at a single Walmart store. When the initial cases first appeared, the local health authorities had no idea they were all linked to one workplace. Once they put the pieces together, they temporarily closed the store. If the public health authorities had known earlier, they could have intervened more quickly and prevented some of the cases.62
Whether through an OSHA Emergency Temporary Standard or Executive Orders issued by governors, employers should be required to promptly notify OSHA of all cases from a workplace in which two or more workers have been found to be infected within a fourteen-day period—whether or not employer thinks the cases are work-related—and alert the state or local health department of any individual case of COVID-19 at that workplace.
Once notified, OSHA should consider whether an inspection is warranted using the same approach applied in considering complaints (see below). However, a cluster of two or more cases is suggestive of the presence of a significant problem.63 As part of its contact tracing activities the local health authority should promptly interview the workers involved, and OSHA and the local health officials should together determine if immediate intervention is appropriate, with local health authorities closing the establishment if an imminent danger is identified.
MSHA, like OSHA, has the ability to mandate case reporting and respond to these reports. It should do so.
4. Encourage Collaborative Workplace Infection Control Efforts
Infection control is not simple or easy and requires the active cooperation of everyone involved. In general, successful hazard control initiatives require worker involvement in all aspects of SHMS programs. This is even more true of an infection control plan; workers have the most to lose if the plan fails, but if they do not have some ownership in the program, it is less likely to succeed. For these reasons, the plan can’t simply be imposed by fiat. It must be developed, implemented, and continuously evaluated with the input and collaboration of the workers, including, if there is one, the workers’ union. One component of such plans should be the provision of paid leave to workers who have developed symptoms or who have been exposed to the virus. This is important for infection control, and also demonstrates the employer’s commitment to the health and safety of its employees.
Employers and workers will need assistance in designing and implementing these plans. OSHA should refocus the OSHA-funded, state-based free consultation programs,64 prioritizing assisting small employers in developing collaborative infection control programs. The OSHA Education Centers65 should also offer courses for managers and workers in infection control, with a small group of Education Centers assigned to develop web-based education and training materials for use by Centers and other non-OSHA educational institutions. Infection control should also be prioritized in an enlarged Susan Harwood worker training grant program.66
5. Increase PPE Production
Incredibly, seven months into the pandemic, nurses and other frontline health care personnel actively treating or caring for COVID-19 patients are still being required to reuse contaminated PPE, including N95 respirators and gowns,67 increasing their own risk of disease. The lack of PPE is particularly acute in nursing homes.68 Early in the pandemic, facing the severe shortage of N95 respirators and under pressure from the hospital industry, the CDC weakened its recommendations for protecting health care workers, claiming that in many situations in which exposure is occurring, surgical masks provide adequate protection.69 There is compelling evidence that N95s are far more protective than surgical masks in preventing COVID-19 transmission in health care settings,70 and it is vitally important that heavily exposed workers be provided with N95s.
While the federal and state governments have spent billions of dollars in attempts to purchase badly needed PPE, these efforts have been scattershot and inadequate, with production contracts given to firms with little experience in manufacturing.71 The result is that the shortage continues, with no end in sight.
The administration needs to make the production of PPE—especially N95 and other more protective respirators—a top national priority and invoke the Defense Production Act to prioritize production of PPE.
The administration needs to make the production of PPE—especially N95 and other more protective respirators—a top national priority and invoke the Defense Production Act to prioritize production of PPE. With the participation of OSHA, NIOSH, CDC, and the Department of Commerce, the White House should immediately convene meetings with manufacturers who either currently or could soon produce needed PPE, and the unions representing workers in those facilities, and together work out a new production schedule, providing subsidies or purchase guarantees, if needed.
6. Change How Inspections Are Done
OSHA’s practice is to conduct workplace inspections following reports of workers being killed, hospitalized, or suffering an amputation; in response to worker complaints; or as part of a program that prioritizes planned preventive inspections at high-hazard workplaces. OSHA’s inspections have two objectives. The first and paramount objective is deterrence: to send a message to all employers that they should eliminate hazards before workers are injured (and before they are inspected and cited by OSHA). The second is to identify and cite employers for hazards at the inspected workplaces so that the employers eliminate them, thus preventing injuries and illness in the future.
Thousands of workers across the nation, fearful they are being exposed at work to COVID-19, have reached out to OSHA asking for help.72 OSHA’s inspections could play a central role in reducing workplace exposures, but the agency is not employing this tool to address the COVID-19 crisis in the workplace, and, as discussed above, the agency’s small fines in the few inspections it has completed to tell employers that they need not fear an OSHA inspection.
When cases of COVID-19 began to appear first among workers in hospital and nursing homes, and then among other groups of heavily exposed workers, OSHA simply did no COVID-19 inspections. It has been reported that OSHA staff told workers who contacted the agency for help that OSHA did not even cover COVID-19.73 In April, OSHA announced it would initiate inspections,74 but only following reports of worker deaths or imminent danger in health care facilities where high-risk procedures were being performed.
In response to these thousands of complaints and to the hundreds of reports of COVID-related deaths and hospitalizations, OSHA has started only a very small number of actual physical inspections, even failing to send inspectors to visit workplaces in which several workers have died and hundreds more have been sickened. The vast majority of “investigations” done in response to complaints and reports of deaths or hospitalizations are closed with, at most, a phone call or letter to the employer. No actual inspection occurred, no citations were issued, and no requirements to protect workers were placed upon the employer.
OSHA does not have the resources to send inspectors to all the workplaces where workers have complained or, sadly, even all workplaces where workers have died from COVID-19. Congress needs to fund a significant increase in OSHA’s small budget to address COVID-19. But in the meantime, OSHA must initiate more and faster on-site inspections in response to complaints in industries that have been and continue to be sources of multiple worker deaths. The agency should develop a system to issue citations within a few weeks after beginning an inspection in those workplaces where the employer fails to provide adequate distancing or PPE. These should be publicized with strong press releases and in press conferences.
OSHA does not have the resources to send inspectors to all the workplaces where workers have complained or, sadly, even all workplaces where workers have died from COVID-19.
For the sites not inspected, simply speaking with some employers on the phone is not sufficient. In response to complaints for which OSHA cannot do a timely inspection, the agency should reach out to the employer and let them know they are expected to abate the hazard and to send OSHA attestation of abatement, or of safe conditions if the employer believes the complaint was not accurate. OSHA should confirm abatement with workers who have filed complaints or their representatives. If an employer fails to address a problem, they should be subject to citation and penalties. As part of this program, OSHA should conduct randomly chosen follow-up on-site inspections to determine the adequacy and effectiveness of employers’ infection control efforts.
One mechanism for achieving workplace change that OSHA has used successfully in the past is to announce that it will start doing random inspections in selected high-hazard industries. This is a powerful motivator for many employers in the industry to take steps to protect their workers, even though only a fraction are actually inspected. To impact more employers, OSHA should use this tool, targeting farms, meat and poultry factories, nursing homes and other workplaces where large numbers of workers have been infected but who may be less likely to send complaints into the agency.
OSHA inspectors issue citations and fines when the inspector finds the establishment is in violation of a standard. These inspections are effective in preventing injuries at that workplace for years after the inspection takes place.75 In normal times, it can take weeks or even months to complete the process necessary to issue the violation. This would be true even if the agency issued an emergency standard, but it is a particularly acute problem now, when there are no COVID-19-related standards in place at all. In the first six months of the pandemic, with thousands of workers sickened by the virus, OSHA issued only a handful of citations, none with a large fine. To lower expectations during the pandemic, the OSHA’s current press office regularly reminds the public that it may take the entire six months allowed by the OSHA law before it will issue a citation.
Citations issued months after a complaint will have little or no impact on the course of the pandemic. Given the crisis, OSHA should not be treating these inspections as business as usual; instead, it should issue citations as quickly as possible. However, unless OSHA issues an ETS requiring employers to protect workers from airborne infectious agents, it will have to rely primarily on the general duty clause: the part of the OSHAct that requires employers to provide workplaces free of “recognized serious hazards.” General duty clause citations require a tremendous amount of work by the OSHA technical staff and attorneys and do often take several months to issue. Once OSHA issues its emergency standard, citations can be issued much more promptly.
Exposures occurring now must be addressed immediately. In addition to prompt OSHA enforcement, if dangerous conditions are found, OSHA should engage the local health department or sheriff’s office to launch a concurrent investigation and use its authority to temporarily close the workplace if the employer doesn’t immediately address conditions identified by the OSHA inspector.
MSHA is mandated to inspect every U.S. mine comprehensively multiple times a year. This agency’s inspection process should be supplemented to include assessment of the adequacy of the design and implementation of COVID-19 prevention plans and compliance with a mandate to report of COVID-19 infections among the mining workforce.
7. Amplify the Impact of Inspections
OSHA’s normal approach to inspections generally results in prompt improvement in conditions at the inspected facilities. However, as discussed above, an important objective of OSHA’s inspections is to impact many employers, not just those inspected, encouraging non-inspected firms to ensure the safety of their workers on the job. Given the enormity of the crisis, OSHA needs to dramatically raise its profile and let employers in every sector know in no uncertain terms that it is their obligation to make sure their workers can work safely.
OSHA has a very powerful tool to increase the deterrent effect of its inspections: by using press releases and social media promotion to publicize the results of those inspections and employer responsibilities, OSHA can inform and persuade many additional employers to make efforts to eliminate workplace hazards. A recent study found that each OSHA press release reporting citations issued after an inspection generates as much compliance with OSHA standards as 210 additional inspections.76 OSHA is currently issuing press releases to announce the results of its few inspections, like the ones at Smithfield Foods and JBS; the problem is that the small size of the penalties sends the opposite message as OSHA should want to convey.
A recent study found that each OSHA press release reporting citations issued after an inspection generated as much compliance with OSHA standards as 210 additional inspections.
To impact employers most widely, OSHA should immediately launch several inspections in high-hazard industries (including nursing homes, farms, and meat factories), publicizing them in a way to get maximum attention. After a day or two of inspecting, the agency should hold a press briefing to notify the nation the reason the inspection was launched. Early press briefings are used by the National Transportation Safety Board when it launches investigations. These briefings generally get regional if not national attention. Although OSHA normally does not speak to the press about ongoing inspections, the importance of changing behavior of many employers rapidly in this pandemic requires new approaches by OSHA.
8. Encourage Innovation in the States
States with their own OSHA programs are far ahead of the federal government in requiring employers to follow the law and provide safe workplaces. Using its Injury and Illness Prevention Program regulation, Cal/OSHA, California’s state plan, has issued fines against host employers and staffing agencies for failing to protect virus-exposed workers many times larger than those imposed by federal OSHA.77 Cal/OSHA also has an aerosol disease standard that covers health care and corrections employees and is now working on a broader COVID-19 emergency standard.78 Washington79 has very clear rules that employers must follow, Virginia80 has issued an ETS, and Oregon81 is poised to do the same.
States without state OSHA plans and therefore without enforcement mechanisms are at a great disadvantage. Still, governors of several of these states are taking steps to increase worker protections.82 While a strong, clear national standard enforced by OSHA would better protect all workers and help firms with multiple locations avoid having to meet different requirements in different states, until federal OSHA steps up to the plate, progressive states will take the lead in protecting workers.
However, even if federal OSHA issues an ETS and improves its own enforcement activities, OSHA should assist states in developing and evaluating new programs to encourage employers to better protect workers.
There are significant gaps in OSHA coverage among non-federal public sector workers. Only the twenty-two OSHA state plans (including Puerto Rico) are required to cover each of those state’s public sector workers; five additional states and the Virgin Islands have OSHA plans for only their own public sector workers. But the remaining 8–9 million public sector workers in twenty-four states and the District of Columbia are employed in OSHA-free zones. OSHA should offer its assistance to labor and public health departments in those states, encouraging them to use public health authority to require state and local government employers to protect workers from COVID-19.83 H.R. 6559 and the HEROES Act would expand coverage under the ETS to all public employees.
States can also take other sorts of actions to protect workers. Ohio Governor Mike DeWine, for example, issued an Executive Order expanding eligibility for unemployment benefits to workers who refuse work because their employer “does not allow the employee to practice social distancing, hygiene, and wearing protective equipment.”84
9. Better Protect Whistleblowers: Encourage Workers to Raise Safety Concerns
Whistleblowers play a vital role in identifying hazards and protecting themselves and their coworkers. Employers should welcome the concerns they raise, because workers are often the first to spot conditions that may result in exposure to themselves, to other workers, or to the public. From the first report of a Washington State physician being fired after raising safety concerns,85 there have been numerous reports of retaliation against workers for raising safety concerns with their employer or with OSHA, or for using their own personal protective equipment when management did not supply adequate protection. Amazon, for example, has retaliated against workers who raised safety concerns, prompting the resignation of a longtime senior executive who described it as a “vein of toxicity running through the company culture.”86 Before CDC recommended that everyone should wear masks in public and at workplaces, workers from security guards to physicians were fired or reprimanded for bringing their own masks to work.
Whistleblowers play a vital role in identifying hazards and protecting themselves and their coworkers.
While unionized workers are more likely to feel sufficiently protected to raise safety concerns,87 more than 90 percent of private sector workers do not have the protection of union membership. The whistleblower protection provisions included in the OSH Act fifty years ago are weak and badly in need of updating.88 Congress has since passed numerous laws containing stronger, more effective whistleblower protection provisions. To better protect workers who raise concerns, OSHA’s COVID-19 emergency standard should include much stronger anti-retaliation language.
OSHA’s current approach to protecting COVID-19 exposed workers who raise safety concerns is tragically inadequate. The OSHA whistleblower protection program is staffed with dedicated professional investigators, but it is small and there is no way they can keep up with the enormous flood of new cases. An investigation by the Department of Labor’s Inspector General found that, by the end of May 2020, more than 1,600 workers filed whistleblower complaints, alleging they had suffered retaliation for raising safety concerns; OSHA quickly dismissed more than half of the complaints.89 At the same time, OSHA’s whistleblower investigation staff was losing staff and getting smaller. The complaints are still pouring in, passing 3,000 by the beginning of September, with no let-up in sight.90
The whistleblower protection process at OSHA has not changed to respond to the challenge of the pandemic: the staff processes cases as they come in and, in some instances, the investigators successfully convince some employers to withdraw the retaliation. But this is done with no publicity, so it has no impact on the behavior of any other employer. There are hundreds—or perhaps thousands—of cases in which protection efforts were not attempted or have failed, and it will be many months before OSHA can even investigate most of these claims. The workers who have already been fired or otherwise penalized will wait years for justice, and the employers involved will, at most, have to withdraw the retaliation and provide lost pay. None will be assessed any additional penalty for their illegal action. And, most important, during all this time, coworkers, customers, and their families and communities could be at risk for COVID-19 transmission.
Even if OSHA issues an emergency standard with strong anti-retaliation provisions, it will be difficult to address the already large and growing backlog of whistleblower claims. These workers need and deserve prompt assistance. To help these workers, the Department of Justice or other agencies should detail teams of investigators to assist OSHA in investigating these claims.
A national public focus on retaliation issues is necessary to bring badly needed improvements at workplaces across the country. To be effective, however, this message must come from the highest levels of the federal government. Very senior federal officials, preferably the president, the vice president, and the secretary of labor, should be a constant presence in traditional and social media, warning employers that retaliation for raising safety concerns is against the law and won’t be tolerated. They should remind employers that workers are the ones at risk, and often know what needs to be done to ensure they are safe.
10. Support Workplace Testing
COVID-19 viral tests are an important tool in maintaining a virus-free workplace and will become more widely used as their accuracy and speed increases and their price drops. Identification of active COVID-19 cases in workplaces, as well as before new workers enter the workplace, not only helps stop virus spread in that workplace but also is a vital component of the larger national effort to stem the pandemic.
As testing improves, the CDC should continue to refine and communicate workplace screening and surveillance testing protocols, assisting employers in prioritizing testing of workers at higher risk of infection or who need to be tested before returning to work. The current cost of this testing is high and the tests may not be easy to acquire, making surveillance and screening especially difficult for small employers. In some locations where states or the federal government has required testing, there is uncertainty and confusion as to who should bear the costs of the testing.91 The federal government, utilizing the infrastructure and payment mechanisms of the Centers for Medicare and Medicaid Services, should subsidize or cover the costs of viral testing, setting reimbursement rates and imposing quality assurance systems on the firms providing the testing.
In addition, having the government fund testing allows the activity to be decoupled from employment status. There are undoubtedly many workers classified as independent contractors or gig workers whose need to be tested is equal to that of workers employed through traditional employment relationships.
11. Develop and Implement a Worker Protection Research Agenda
Adequate worker protections must be based on the best available science. Under the OSH Act, NIOSH is charged with working closely with OSHA to understand workplace risks and develop effective responses to them. NIOSH staff have a wealth of expertise in evaluating workplace hazards, developing control technologies to mitigate the hazards, and analyzing and reporting the distribution of diseases and injuries across different working populations. NIOSH is also responsible for testing, certifying, and auditing respiratory protective equipment such as N95 and other respirators.
Adequate worker protections must be based on the best available science.
NIOSH has done important work during the pandemic, including developing a low-cost way to isolate infected patients using a negative pressure bed headboard and clear “tent” over patient beds. But there is much more it could be doing, given the resources and opportunity. For example, concerns about the risk to teachers and students of classrooms with inadequate ventilation could be addressed by NIOSH research and guidance. If industry and occupation were included in the electronic medical records of everyone seen by a doctor for COVID-19, hospitalized with COVID-19, or who has died from the disease, we would be able to identify workplace “hot spots” and intervene quickly to reduce spread. Research to develop better-fitting, lower-cost protective respirators using modern imaging and scanning technologies would be helpful, as would be an expansion of the capacity to test, certify, and audit the production of the current crop of existing and new respirators and other protective equipment.
Continuing response to the pandemic and preparation for the next emerging hazard requires maintenance of a sophisticated focused scientific capability. A research agenda can and should be developed with this in mind and the resources—human, financial, and material—provided to translate the agenda into reality. Public health is most effective when problems are anticipated, solutions are developed and tested, and the adequacy of the solutions and interventions are monitored and then adjusted to assure the best protections. Each step in the prevention process requires high quality credible scientific work engaging a wide range of disciplines.
Conclusion
The COVID-19 crisis has illuminated the vital role that workers—particularly many previously invisible low-wage workers—play in maintaining the well-being of the country. The importance of a safe and healthy workforce could not be clearer. Yet the crisis has also demonstrated the severe weakness of our system of worker protections. The government devotes far too few resources to ensuring the safety and health of its greatest resource: the nation’s workers. In the immediate future, OSHA desperately needs far more resources. Congress should firmly reject annual attacks on OSHA’s budget and allocate funds to make the agency several times larger than it is at present. Increased staffing alone, however, is not sufficient to make OSHA the effective agency the nation so badly needs. Fifty years after passage of the OSH Act, OSHA needs to be re-imagined and strengthened to address the changes in work, work relations, and the workforce that have occurred over the past several decades.92
The failure of the White House to fully and aggressively utilize the authority of the federal government is one of the reasons that many thousands of workers have been infected with—and hundreds have died from—COVID-19. And, unless both the federal government as a whole and OSHA specifically change course and take bold and creative steps immediately, this failure will result in many more workers dying, setting back efforts to stem the pandemic and restoring social and economic functioning.
Much can and must be done immediately by OSHA and the administration in order to prevent more COVID-19-caused carnage. However, once the pandemic is controlled, we must use the lessons of this disaster to ensure that workers in the future are safe, and that every worker is able to go to work, do their job, and leave at the end of their shift safe and healthy.
Acknowledgments
The authors are grateful to the McElhattan Foundation for its support for this effort. In addition, the authors would like to thank Jordan Barab, Debbie Berkowitz, Earl Dotter, Eric Frumin, Molly Kinder, Jason Renker, Peg Seminario, Patricia Smith, Emily Spieler, and Michael Wright for their comments and assistance in preparing this report.
Notes
- “COVID-19 Nursing Home Dataset,” Centers for Medicare and Medicaid Services, September 17, 2020, https://data.cms.gov/Special-Programs-Initiatives-COVID-19-Nursing-Home/COVID-19-Nursing-Home-Dataset/s2uc-8wxp
- “Coronavirus disease 2019 (COVID-19): Cases in the U.S.,” U.S. Centers for Disease Control and Prevention, https://tinyurl.com/yx8jcx72
- “The COVID Racial Data Tracker,” The COVID Tracking Project, https://covidtracking.com/race.
- Chris Kirkham and Benjamin Lesser, “Special Report: Pandemic exposes systemic staffing problems at U.S. nursing homes,” Reuters, June 10, 2020, https://tinyurl.com/ydhmn6zt
- Brian E. McGarry, David C. Grabowski, and Michael L. Barnett, “Severe Staffing and Personal Protective Equipment Shortages Faced by Nursing Homes during the COVID-19 Pandemic,” Health Affairs, August 20, 2020, https://doi.org/10.1377/hlthaff.2020.01269; Jordan Rau, “Federal Help Falters as Nursing Homes Run Short Of Protective Equipment,” Kaiser Health News, June 11, 2020, https://khn.org/news/federal-help-falters-as-nursing-homes-run-short-of-protective-equipment/.
- “Purdue Food and Agriculture Vulnerability Index,” Purdue University, https://ag.purdue.edu/agecon/Pages/FoodandAgVulnerabilityIndex.aspx.
- Polly Mosendz, Peter Waldman, and Lydia Mulvany, “U.S. Meat Plants Are Deadly as Ever, With No Incentive to Change,” Bloomberg Businessweek, June 18, 2020, https://www.bloomberg.com/news/features/2020-06-18/how-meat-plants-were-allowed-to-become-coronavirus-hot-spots?sref=w8mEqFdc
- Michael A. Waltenburg et al., “Update: COVID-19 Among Workers in Meat and Poultry Processing Facilities―United States, April–May 2020,” Morbidity and Mortality Weekly Report 69, no. 27 (July 10, 2020), http://dx.doi.org/10.15585/mmwr.mm6927e2.
- Leah Douglass, “Mapping Covid-19 outbreaks in the food system,” Food and Environment Reporting Network, April 22, 2020, https://thefern.org/2020/04/mapping-covid-19-in-meat-and-food-processing-plants/.
- Lois Beckett, “Revealed: Nearly 100 US Transit Workers have Died of COVID-19 Amid Lack of Basic Protections,” The Guardian, April 20, 2020, https://www.theguardian.com/world/2020/apr/20/us-bus-drivers-lack-life-saving-basic-protections-transit-worker-deaths-coronavirus
- Eduardo Hernandez, “’We do not have the Luxury to Work from Home’: The Impact of COVID-19 on Illinois’ Essential Temp Workforce,” Chicago Workers’ Collaborative, September, 2020, https://www.chicagoworkerscollaborative.org/coronavirus-survey
- Elise Gould and Valerie Wilson, “Black Workers Face Two of the Most Lethal Preexisting Conditions for Coronavirus—Racism and Economic Inequality,” Economic Policy Institute, June 1, 2020, https://www.epi.org/publication/black-workers-covid/
- Grace McCormack, Christopher Avery, Ariella Kahn-Lang Spitzer, and Amitabh Chandra, “Economic vulnerability of households with essential workers,” Journal of the American Medical Association, June 18, 2020, https://jamanetwork.com/journals/jama/fullarticle/2767630
- Steve Karnowski, “Some blame meatpacking workers, not plants, for virus spread,” Associated Press, May 8, 2020, https://www.startribune.com/some-blame-meatpacking-workers-not-plants-for-virus-spread/570307012/
- Deborah Berkowitz “Worker Safety In Crisis: The Cost of a Weakened OSHA,” National Employment Law Project, April 28, 2020, https://www.nelp.org/publication/worker-safety-crisis-cost-weakened-osha/.
- David Michaels, “Adding Inequality to Injury: The Costs of Failing to Protect Workers on the Job,” U.S. Occupational Safety and Health Administration, June, 2015, https://www.osha.gov/Publications/inequality_michaels_june2015.pdf.
- Philip Bump, “ Prisons and meat processors are hotbeds of coronavirus. One can’t close. The other won’t be allowed to.” Washington Post, April 28, 2020, https://www.washingtonpost.com/politics/2020/04/28/prisons-meat-processors-are-hotbeds-coronavirus-one-cant-close-other-wont-be-allowed/
- David Michaels and Gregory R. Wagner, “Occupational Safety and Health Administration (OSHA) and Worker Safety During the COVID-19 Pandemic,” Journal of the American Medical Association, September 16, 2020, https://jamanetwork.com/journals/jama/fullarticle/2770890.
- “OSH Act of 1970,” Occupational Safety and Health Administration, December 29, 1970, https://www.osha.gov/laws-regs/oshact/toc.
- David Michaels, “What Trump Could Do Right Now to Keep Workers Safe From the Coronavirus,” The Atlantic, March 2, 2020, https://www.theatlantic.com/ideas/archive/2020/03/use-osha-help-stem-covid-19-pandemic/607312/.
- “Meat and Poultry Processing Workers and Employers,” Centers for Disease Control, July 9, 2020, https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/meat-poultry-processing-workers-employers.html.
- David Michaels, “Testimony of Assistant Secretary Dr. David Michaels before the House Committee on Education and the Workforce Subcommittee on Workforce,” Occupational Safety and Health Administration, October 7, 2015, https://www.osha.gov/news/testimonies/10072015.
- David I. Levine, Michael W. Toffel, and Matthew S. Johnson, “Randomized government safety inspections reduce worker injuries with no detectable job loss,” Science 336, no. 6083, May 18, 2012, https://science.sciencemag.org/content/336/6083/907. ; see also David Michaels, “OSHA does not kill jobs: It helps prevent jobs from killing workers,” American Journal of Industrial Medicine 55, no. 11, November 2012, https://doi.org/10.1002/ajim.22122
- Bob Brigham, “Republican claims people will be forced to wear masks in the shower if ‘Heroes Act’ passes,” Raw Story, May 12, 2020, https://www.rawstory.com/2020/05/republican-claims-people-will-be-forced-to-wear-masks-in-the-shower-if-heroes-act-passes/.
- “Injuries, Illnesses, and Fatalities,” August 4, 2020, Bureau of Labor Statistics, https://www.bls.gov/iif/data-quality.htm.
- Jukka Takala et al., “Global Estimates of the Burden of Injury and Illness at Work in 2012,” Journal of Occupational and Environmental Hygiene, May, 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4003859/.
- Deborah Berkowitz, “Worker Safety in Crisis: The Cost of a Weakened OSHA,” National Employment Law Program, April 28, 2020, https://www.nelp.org/publication/worker-safety-crisis-cost-weakened-osha/.
- Polly Mosendz, Peter Waldman, and Lydia Mulvany, “U.S. Meat Plants Are Deadly as Ever, With No Incentive to Change,” Bloomberg Businessweek, June 18, 2020, https://www.bloomberg.com/news/features/2020-06-18/how-meat-plants-were-allowed-to-become-coronavirus-hot-spots?sref=w8mEqFdc
- “Executive Order on Delegating Authority Under the DPA with Respect to Food Supply Chain Resources During the National Emergency Caused by the Outbreak of COVID-19,” The White House, April 28, 2020, https://www.whitehouse.gov/presidential-actions/executive-order-delegating-authority-dpa-respect-food-supply-chain-resources-national-emergency-caused-outbreak-covid-19/.
- Michael Grabell and Bernice Yueng, “Emails Show the Meatpacking Industry Drafted an Executive Order to Keep Plants Open,” ProPublica, September 14, 2020, https://www.propublica.org/article/emails-show-the-meatpacking-industry-drafted-an-executive-order-to-keep-plants-open.
- “U.S. Department of Labor Cites Smithfield Packaged Meats Corp. for Failing To Protect Employees from Coronavirus,” U.S. Department of Labor, September 10, 2020, https://www.dol.gov/newsroom/releases/osha/osha20200910.
- “U.S. Department of Labor Cites JBS Foods Inc. for Failing to Protect Employees from Exposure to the Coronavirus,” news release, U.S. Department of Labor, September 11, 2020, https://www.dol.gov/newsroom/releases/osha/osha20200911-1.
- “OSHA embarrasses itself, re-lights bitter fires with late, low fine of JBS,” editorial, Greeley Tribune, September 12, 2020, https://www.greeleytribune.com/2020/09/12/editorial-osha-embarrasses-itself-re-lights-bitter-fires-with-late-low-fine-of-jbs/.
- Dillon Tomas, “’It’s a Joke’: Family Reacts to $15,000 Fine Against Greeley’s JBS Plant,” CBS Denver, September 13, 2020, https://denver.cbslocal.com/2020/09/13/saul-sanchez-jbs-greeley-fine-coronavirus/
- “Top Enforcement Cases Based on Total Issued Penalty,” Occupational Safety and Health Administration, https://www.osha.gov/dep/enforcement/top_cases.html.
- “Top Enforcement Cases Based on Total Issued Penalty,” Occupational Safety and Health Administration, https://www.osha.gov/dep/enforcement/top_cases.html.
- Shayla Thompson and Deborah Berkowitz, “USDA Allows Poultry Plants to Raise Line Speeds, Exacerbating Risk of COVID-19 Outbreaks and Injury,” National Employment Law Project, June 17, 2020, https://www.nelp.org/publication/usda-allows-poultry-plants-raise-line-speeds-exacerbating-risk-covid-19-outbreaks-injury/.
- Sam Mintz, “Chao cool on ‘heavy-handed’ pandemic regulations for airlines,” POLITICO, June 3, 2020, https://www.politico.com/news/2020/06/03/transportation-secretary-pandemic-airline-regulations-298522.
- “Safe to Work Act,” S. 4317, 116th Congress, July 27, 2020, https://www.congress.gov/bill/116th-congress/senate-bill/4317/all-info.
- “Opening Up America Again,” The White House, https://www.whitehouse.gov/openingamerica/.
- “US Labor Department and Federal Communications Commission Announce Working Group to Prevent Fatalities in Telecommunications Industry,” news release, U.S. Department of Labor, October 14, 2014, https://www.dol.gov/newsroom/releases/osha/osha20141014.
- David Michaels and Gregory Wagner, “Occupational Safety and Health Administration (OSHA) and Worker Safety During the COVID-19 Pandemic,” Journal of the American Medical Association, September 16, 2020, https://jamanetwork.com/journals/jama/fullarticle/2770890
- “Workplace Safety and Health: Multiple Challenges Lengthen OSHA’s Standard Setting,” U.S. Government Accountability Office, April 2, 2012, https://www.gao.gov/products/GAO-12-330.
- David Michaels, “What Trump Could Do Right Now to Keep Workers Safe From the Coronavirus,” The Atlantic, March 2, 2020, https://www.theatlantic.com/ideas/archive/2020/03/use-osha-help-stem-covid-19-pandemic/607312/.
- “OSH Act of 1970, Sec. 6,” Occupational Safety and Health Standards, December 29, 1970, https://www.osha.gov/laws-regs/oshact/section_6.
- The workers not under OSHA’s authority, and therefore not covered by an emergency standard issued by OSHA, include underground and surface miners (covered by MSHA), some transportation workers (covered by various Department of Transportation agencies), and public sector workers in twenty-four states who have no OSHA coverage at all.
- See, for example, “Hierarchy of Controls,” Centers for Disease Control and Prevention, https://www.cdc.gov/niosh/topics/hierarchy/default.html.
- U.S. Department of Labor Press Release, April 26, 2020, https://www.dol.gov/newsroom/releases/osha/osha20200426-0
- “A Petition to Secretary Scalia for an OSHA Emergency Temporary Standard for Infectious Disease,” AFL–CIO, March 6, 2020, https://aflcio.org/statements/petition-secretary-scalia-osha-emergency-temporary-standard-infectious-disease.
- Letter from Secretary of Labor Eugene Scalia to Richard L. Trumka, president, AFL–CIO, April 30, 2020, https://aboutblaw.com/Qzv.
- “COVID-19: Control and Prevention: Interim guidance for specific worker groups and their employers,” Occupational Safety and Health Administration, https://www.osha.gov/SLTC/covid-19/controlprevention.html#interim
- “Guidance on Returning to Work,” Occupational Safety and Health Administration, OSHA 4045-06 2020, https://www.osha.gov/Publications/OSHA4045.pdf.
- Sang Hyun Ra, et al., “Upper Respiratory Viral Load in Asymptomatic Individuals and Mildly Symptomatic Patients with SARS-CoV-2 Infection,” Thorax Epub, September 22, 2020, http://press.psprings.co.uk/thx/september/thx215042.pdf
- “Recommended Practices for Safety and Health Programs,” Occupational Safety and Health Administration, https://www.osha.gov/shpguidelines/.
- “The COVID-19 Every Worker Protection Act of 2020 H.R. 6559,” House Committee on Education and Labor, April 21, 2020, https://edlabor.house.gov/imo/media/doc/2020-04-21%20The%20COVID19%20Every%20Worker%20Protection%20Act%20Fact%20Sheet.pdf.
- “Enforcement Guidance for Recording Cases of Coronavirus Disease 2019 (COVID-19),” Occupational Safety and Health Administration, April 10, 2020, https://www.osha.gov/memos/2020-04-10/enforcement-guidance-recording-cases-coronavirus-disease-2019-covid-19.
- “Revised Enforcement Guidance for Recording Cases of Coronavirus Disease 2019 (COVID-19),” Occupational Safety and Health Administration, May 19, 2020, https://www.osha.gov/memos/2020-05-19/revised-enforcement-guidance-recording-cases-coronavirus-disease-2019-covid-19.
- “Occupational Injury and Illness Recording and Reporting Requirements–NAICS Update and Reporting Revisions; Final Rule, Federal Register 79 , no. 181 (September 18, 2014), https://www.govinfo.gov/content/pkg/FR-2014-09-18/html/2014-21514.htm
- “Revised Enforcement Guidance for Recording Cases of Coronavirus Disease 2019 (COVID-19),” Occupational Safety and Health Administration, May 19, 2020, https://www.osha.gov/memos/2020-05-19/revised-enforcement-guidance-recording-cases-coronavirus-disease-2019-covid-19.
- “U.S. Department of Labor Issues Frequently Asked Questions and Answers About Reporting Work-Related Cases of the Coronavirus,” Occupational Safety and Health Administration, September 30, 2020, https://www.osha.gov/news/newsreleases/national/09302020
- “Update to the Standardized Surveillance Case Definition and National Notification for 2019 Novel Coronavirus Disease (COVID-19),” Council of State and Territorial Epidemiologists, https://cdn.ymaws.com/www.cste.org/resource/resmgr/ps/positionstatement2020/Interim-20-ID-02_COVID-19.pdf.
- Janelle Nanos, “How a Walmart in Worcester became a coronavirus hot spot,” Boston Globe, May 5, 2020, https://www.bostonglobe.com/2020/05/05/business/how-walmart-worcester-became-coronavirus-hot-spot/.
- “Update to the Standardized Surveillance Case Definition and National Notification for 2019 Novel Coronavirus Disease (COVID-19),” Council of State and Territorial Epidemiologists, https://cdn.ymaws.com/www.cste.org/resource/resmgr/ps/positionstatement2020/Interim-20-ID-02_COVID-19.pdf.
- “On-Site Consultation,” Occupational Safety and Health Administration, https://www.osha.gov/consultation.
- “OSHA Training Institute Education Centers,” Occupational Safety and Health Administration, https://www.osha.gov/otiec/.
- “Susan Harwood Training Grants,” Occupational Safety and Health Administration, https://www.osha.gov/harwoodgrants.
- Jordan Rau, “Federal Help Falters as Nursing Homes Run Short Of Protective Equipment,” Kaiser Health News, June 11, 2020, https://khn.org/news/federal-help-falters-as-nursing-homes-run-short-of-protective-equipment/.
- Brian E. McGarry, David C. Grabowski, and Michael L. Barnett, “Severe Staffing and Personal Protective Equipment Shortages Faced by Nursing Homes during the COVID-19 Pandemic,” Health Affairs, August 20, 2020, https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.01269.
- Jennifer Gollan and Elizabeth Shogren, “31,000 and counting,” Reveal, May 11, 2020, https://www.revealnews.org/article/31000-and-counting/.
- Raina MacIntyre and Quanyi Wang, “Physical distancing, face masks, and eye protection for prevention of COVID-19,” The Lancet, June 1, 2020, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31183-1/fulltext.
- Cheryl W. Thompson, Joel Rose, and Robert Benincasa, “Feds Spend Billions on COVID-19 Contracts, Often Without Fully Competitive Bidding,” National Public Radio, June 9, 2020, https://www.npr.org/2020/06/09/869052415/feds-spend-billions-on-covid-19-contracts-often-without-fully-competitive-biddin.
- Peter Whoriskey, Jeff Stein, and Nate Jones, “Thousands of OSHA complaints filed against companies for virus workplace safety concerns, records show,” Washington Post, April 16, 2020, https://www.washingtonpost.com/business/2020/04/16/osha-coronavirus-complaints/.
- Meghan Bobrowsky “‘OSHA is AWOL’: Critics say federal agency is where workplace COVID-19 complaints go to die,” Miami Herald, July 3, 2020, https://www.miamiherald.com/news/coronavirus/article243816822.html.
- “Interim Enforcement Response Plan for Coronavirus Disease 2019 (COVID-19),” Occupational Safety and Health Administration, April 13, 2020, https://www.osha.gov/memos/2020-04-13/interim-enforcement-response-plan-coronavirus-disease-2019-covid-19.
- David I. Levine, Michael W. Toffel, and Matthew S. Johnson, “Randomized government safety inspections reduce worker injuries with no detectable job loss,” Science 336, no. 6083 (May 18, 2012), https://science.sciencemag.org/content/336/6083/907; see also David Michaels, “OSHA does not kill jobs: It helps prevent jobs from killing workers,” American Journal of Industrial Medicine 55, no. 11 (November 2012), https://doi.org/10.1002/ajim.22122.
- Matthew S. Johnson, “Regulation by Shaming: Deterrence Effects of Publicizing Violations of Workplace Safety and Health Laws,” American Economic Review 10, no. 6 (June 2020), https://www.aeaweb.org/articles?id=10.1257/aer.20180501&&from=f.
- “Cal/OSHA Cites Frozen Food Manufacturer, Staffing Firm for Failing to Protect Hundreds of Workers from COVID-19,” Cal/OSHA news release, September 9, 2020, https://www.dir.ca.gov/DIRNews/2020/2020-78.html.
- Jie Jenny Zou, “Cal/OSHA will Create Emergency COVID Workplace Safety Rules,” Los Angeles Times, September 17, 2020, https://www.latimes.com/politics/story/2020-09-17/covid-19-cal-osha-workplace-safety-rules.
- “Coronavirus (COVID-19) Prevention: General Requirements and Prevention Ideas for Workplaces,” Washington State Department of Labor and Industries, Division of Occupational Safety and Health, https://lni.wa.gov/forms-publications/F414-164-000.pdf?utm_medium=email&utm_source=govdelivery.
- “Infectious Disease Prevention: SARS-CoV-2 Virus That Causes COVID-19 as Adopted by the
Safety and Health Codes Board,” Virginia Department of Labor and Industry, July 15, 2020, https://www.doli.virginia.gov/wp-content/uploads/2020/07/RIS-filed-RTD-Final-ETS-7.24.2020.pdf. - “Infectious Disease Rulemaking,” Oregon OSHA, https://osha.oregon.gov/rules/advisory/infectiousdisease/Pages/default.aspx.
- Deborah Berkowitz, “Which States and Cities Have Adopted Comprehensive COVID-19 Worker Protections?” National Law Employment Project, August 10, 2020, https://www.nelp.org/blog/which-states-cities-have-adopted-comprehensive-covid-19-worker-protections/.
- Passage of H.R. 6559 would provide federal OSHA coverage related to COVID-19 to state and municipal workers in states where they currently have no OSHA coverage.
- Mike DeWine, “Unemployment Insurance During COVID-19 Pandemic,” State of Ohio Executive Order 2020-24D, June 16, 2020, https://content.govdelivery.com/attachments/OHOOD/2020/06/18/file_attachments/1477128/Signed%20Executive%20Order%202020-24D.pdf
- Ron Judd, “Backed by ACLU, whistleblowing doctor sues Bellingham hospital after he was fired for raising coronavirus concerns,” Seattle Times, May 28, 2020, https://www.seattletimes.com/seattle-news/aclu-joins-ousted-doctor-ming-lin-in-lawsuit-against-bellingham-hospital/.
- Tim Bray, “Bye, Amazon,” April 29, 2020, https://www.tbray.org/ongoing/When/202x/2020/04/29/Leaving-Amazon.
- Aaron Sojourner, “Unionized workers are more likely to assert their right to a safe and healthy workplace,”
The Conversation, September 2, 2020, https://theconversation.com/unionized-workers-are-more-likely-to-assert-their-right-to-a-safe-and-healthy-workplace-144718. - “Testimony of Dr. David Michaels,” Assistant Secretary, before the Senate Subcommittee on Employment and Workplace Safety Committee on Health, Education, Labor and Pensions, April 29, 2014, https://www.osha.gov/news/testimonies/04292014. Emily A. Spieler, “Whistleblowers and Safety at Work: An Analysis of Section 11(c) of the Occupational Safety and Health Act,” ABA Journal on Labor and Employment Law 32, no. 1 (Fall 2016): 1–24.
- “COVID-19: OSHA Needs to Improve its Handling of Whistleblower Complaints During the Pandemic,” U.S. Department of Labor, August 14, 2020, https://www.oig.dol.gov/public/reports/oa/viewpdf.php?r=19-20-010-10-105&y=2020.;Deborah Berkowitz, “OSHA Must Protect Whistleblowers Who File Retaliation Complaints,” National Employment Law Program, October 8, 2020, https://www.nelp.org/publication/osha-failed-protect-whistleblowers-filed-covid-retaliation-complaints/.
- See redacted reports list at https://www.osha.gov/sites/default/files/COVID-19_OSHA_WB_Complaints_Report_01.01.20-09.07.20_Redacted.pdf.
- Katie Thomas “Testing Nursing Home Workers Can Help Stop Coronavirus. But Who Should Pay?” New York Times, June 9, 2020, https://www.nytimes.com/2020/06/09/health/testing-coronavirus-nursing-homes-workers.html.
- David Michaels and Jordan Barab, “The Occupational Safety and Health Administration at 50: Protecting Workers in a Changing Economy,” American Journal of Public Health, May 2020, https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2020.305597.











